Prevention | Risk Factors | Screening | Symptoms | Diagnosis | Staging | Prognosis | Treatment | Support
| What is bowel cancer?
Bowel cancer, also known as colorectal cancer, can affect any part of the colon or rectum; it may also be referred to as colon cancer or rectal cancer, depending on where the cancer is located.
The colon and rectum are parts of the large intestine.
The colon is the longest part of the large intestine (the first 1.8 metres). It receives almost completely digested food from the ceacum (a pouch within the abdominal cavity that is considered to be the beginning of the large intestine), absorbs water and nutrients, and passes waste (stool/faeces/poo) to the rectum.
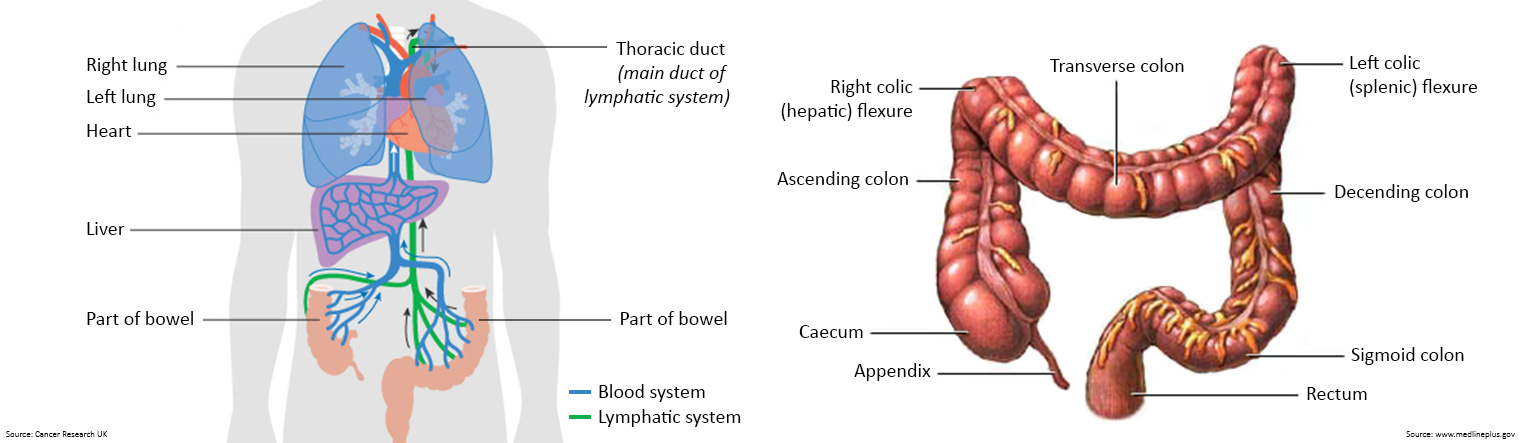
The colon is divided into four parts:
- the ascending colon is the start of the colon. It is on the right side of the abdomen. It continues upward to a bend in the colon called the hepatic flexure.
- the transverse colon follows the ascending colon and hepatic flexure. It lies across the upper part of the abdomen. It ends with a bend in the colon called the splenic flexure.
- the descending colon follows the transverse colon and splenic flexure. It is on the left side of the abdomen.
- the sigmoid colon is the last part of the colon and connects to the rectum.
The proximal colon is the ascending colon and the transverse colon together. The distal colon is the descending colon and the sigmoid colon together.
The rectum is lower part of the large intestine (the last 15 centimetres) that connects to the sigmoid colon. It receives waste (stool/faeces/poo) from the colon and stores it until it passes out of the body through the anus.
The anus is the opening at the lower end of the rectum through which waste is passed from the body.
Cancer in the anal canal or anus is treated differently from and is less common than bowel cancer.
| What are bowel polyps?
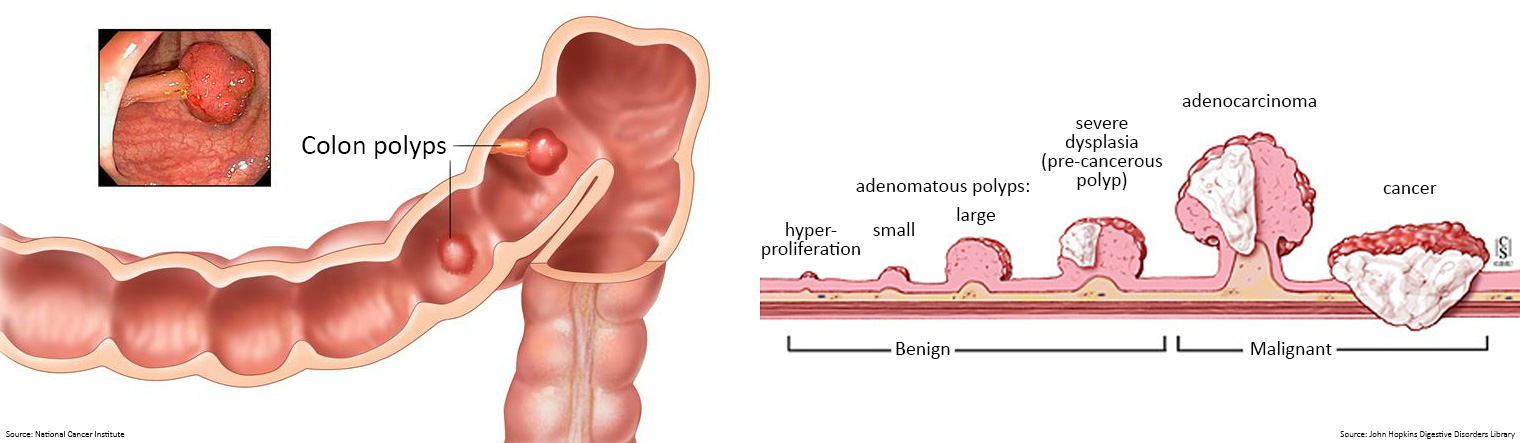
Most bowel cancers start as benign, non-threatening growths – called polyps – on the wall or lining of the bowel.
Polyps typically grow in two shapes: flat or with a stalk. They can vary in size, ranging from a couple of millimeters to several centimetres.
Polyps are fairly common. Around 15-40% of adults have polyps. They are more common in men and older adults.
Polyps are usually harmless; however, adenomatous polyps can become cancerous (malignant) and if left undetected, can develop over time into a cancerous tumour.
The most common type of bowel cancer is called an adenocarcinoma, named after the gland cells in the lining of the bowel where the cancer first develops. Other rarer types include squamous cell cancers (which start in the skin-like cells of the bowel lining), carcinoid tumours, sarcomas and lymphomas.
In advanced cases, the cancerous tumour can spread (metastasise) beyond the bowel to other organs.
Types of bowel polyps
Some polyps grow flat and project outward from a broad base. Others can be depressed, or project inward into the lining of the bowel. Doctors refer to these as sessile polyps.
Pedunculated polyps, on the other hand, may appear raised, projecting out into the hollow centre of the bowel. They may grow in the shape of a small cauliflower or mushroom suspended from a stalk or base.
Adenomas typically have three growth patterns: tubular, villous, and tubulovillous.
- Tubular adenomas are the most common type of bowel polyps, and usually account for 80% of all adenomatous polyps. Tubular adenomas are typically small pedunculated polyps, less than 1.2 centimetres in size. They usually have a tube-like or rounded shape. Tubular adenomas generally take years to form. Typically, the larger the polyp, the greater the risk it may become cancerous.
- Villous adenomas are generally larger pedunculated polyps and grow in a cauliflower-like shape. The term 'villous features' refers to the finger-like or leaf-like projections. Villous adenomas are more likely to become cancerous. They account for 5-15% of all adenomatous polyps.
- Tubulovillous adenomas contain a mixture of tubular and villous growth. They usually have 25-75% villous features, and they account for roughly 5-15% of all adenomatous polyps.
- Serrated adenomas contain tissues with a sawtooth look. There are two types: sessile serrated adenomas and traditional serrated adenomas. Most serrated adenomas are sessile and resemble small raised bumps. Sessile serrated polyps tend to carry a low risk of becoming cancerous as long as they do not contain major cellular changes. Traditional, or non-sessile, serrated adenomas are rarer and typically pedunculated. They carry a high risk of becoming cancerous.
- Hyperplastic polyps are typically benign, and they are not usually a cause for concern. They will rarely become cancerous, as they have a low malignancy potential.
- Inflammatory polyps occur most often in people with inflammatory bowel disease, such as Crohn’s disease or ulcerative colitis. Some people may also refer to these as pseudopolyps, as they are not true polyps but a reaction to inflammation in the colon. Inflammatory polyps are usually benign and generally do not carry the risk of developing into bowel cancer.
| Who gets bowel cancer?
Bowel cancer affects men and women, young and old.
Australia has one of the highest rates of bowel cancer in the world; 1 in 15 Australians will develop the disease in their lifetime.
Bowel cancer is Australia's second deadliest cancer.
Around 30% people who develop bowel cancer have either a hereditary contribution, family history or a combination of both. The other 70% of people have no family history of the disease and no hereditary contribution.
The risk of developing bowel cancer rises sharply and progressively from age 50, but the number of Australians under age 50 diagnosed with bowel cancer has been increasing steadily. That’s why it’s important to know the symptoms of bowel cancer and have them investigated if they persist for more than two weeks.
Almost 99% of bowel cancer cases can be treated successfully when detected early.
During the early stages of bowel cancer, people may have no symptoms, which is why screening is so important.
As a cancerous tumour grows, it can narrow and block the bowel resulting in changes to the size, shape, and/or colour of poo, with our without rectal bleeding. These symptoms are often attributed to haemorrhoids or simply ignored.
Cancers occurring in the left side of the colon generally cause constipation alternating with diarrhoea, abdominal pain and obstructive symptoms, such as nausea and vomiting.
Right-sided colon lesions produce vague, abdominal aching, unlike the colicky pain seen with obstructive left-sided lesions.
Anaemia (low red blood cell count) resulting from chronic blood loss, weakness, weight loss and/or an abdominal mass may also occur when bowel cancer affects the right side of the colon.
Patients with cancer of the rectum may present with a change in bowel movements; rectal fullness, urgency, or bleeding; and tenesmus (cramping rectal pain).
Any of the below symptoms could be indicative of colon or rectal cancer and should be investigated by your GP if they persist for more than two weeks.
- Blood in your poo or rectal bleeding
- A recent, persistent change in bowel habit (e.g. diarrhoea, constipation or the feeling or incomplete emptying)
- A change in the shape or appearance of your poo (e.g. narrower poos or mucus in poo)
- Abdominal pain or swelling
- Pain or a lump in the anus or rectum
- Unexplained anaemia causing tiredness, weakness or weight loss
There are two kinds of risk factors for bowel cancer – those that can be changed (modifiable) and those that cannot (non-modifiable).
Bowel cancer risk is increased by smoking, eating an excessive amount of red meat (especially when charred), eating processed meats (smoked, cured, salted or preserved), drinking alcohol, and being overweight or obese.
These risks can all be addressed through diet and lifestyle changes and are referred to as modifiable.
Age, family history, hereditary conditions and personal health history can also influence bowel cancer risk. Because they cannot be changed they are referred to as non-modifiable.
People with certain diseases and illnesses seem to be more prone to developing bowel cancer.
These include Type II diabetes, other forms of closely linked cancer such as ovarian or digestive system cancers, and inflammatory bowel diseases (IBD) including Crohn’s and Ulcerative Colitis.
A person’s risk category also depends on how many close relatives have bowel cancer and their age at diagnosis.
Someone with several close relatives diagnosed with bowel cancer before age 50 has a much higher risk than someone with no close relatives with bowel cancer.
In some family members, bowel cancer develops due to an inherited gene mutation. Some of these cause specific conditions, such as Lynch syndrome, Familial Adenomatous Polyposis (FAP), or Attenuated Familial Adenomatous Polyposis.
Diet & lifestyle
Healthy diet and lifestyle choices, as well as screening and surveillance, can help to reduce your bowel cancer risk.
Evidence reveals quitting smoking, abstaining from or limiting alcohol consumption, and eating foods containing dietary fibre are all beneficial.
Maintaining a healthy weight and engaging in regular physical activity have also been shown to reduce the risk of colon cancer, but not rectal cancer.
Additionally, people who are more physically active before a bowel cancer diagnosis are less likely to die from the disease than those who are less active.
For people aged 50-70 years without symptoms or a family history of bowel cancer, a GP may also recommend taking a low dose of aspirin for at least 2.5 years.
Whether or not a person should take aspirin depends on their general health, and whether they have another condition that could be made worse by aspirin (e.g. allergy to aspirin, stomach ulcers, bleeding or kidney problems).
Bowel Cancer Australia recommends participating in screening appropriate to your personal level of risk.
Bowel cancer screening is safe and easy and can be done at home.
For people at average or near average risk* of bowel cancer, Australian medical guidelines recommend screening using a faecal immunochemical test (FIT) every 2 years between ages 45-74.
The guidelines also state GPs can offer a faecal immunochemical test every 2 years to people aged 40-44 who request it, after being fully informed of the benefits (and any possible harms) of testing.
Similarly, the guidelines state a healthcare professional could consider offering a faecal immunochemical test every 2 years to people aged 75-85 who are fit, well and healthy and request screening, after being fully informed of the benefits and potential harms of testing.
Screening involves collecting small samples of toilet water or poo, placing them on a card or in a container, and mailing them to a pathology laboratory for analysis. The results are then sent back to the individual and their GP.
Currently, eligible people aged 50-74 will receive a tax-payer funded faecal immunochemical test (FIT) in the mail from the National Bowel Cancer Screening Program (NBCSP) and asked to take two separate poo samples before sending the completed test back to the laboratory for analysis.
From 1 July 2024, the eligible screening age for the NBCSP will be lowered from 50 to 45.
- Eligible people aged 45-49 can request their first bowel cancer screening test be mailed to them.
- Eligible people aged 50-74 will continue to receive a bowel cancer screening in the mail every 2 years.
All eligible people aged 45-74 can also ask their GP about getting a screening test.
The next test will automatically be mailed every 2 years after your last screening test is completed.
A positive result means blood in poo has been detected. It does not necessarily mean bowel cancer is present but does require further investigation by a GP and a referral for colonoscopy within 30 days.
A negative result means blood in poo has not been detected in the samples; however, it does not guarantee no cancer is present or that the person will never develop bowel cancer.
The at-home test is able to detect non-visible blood that cannot be seen with the naked eye. Blood in poo is one possible symptom of bowel cancer. If the result of the test is positive, the person is contacted to arrange a colonoscopy.
For people ineligible to participate in the government program, talk to your GP or pharmacist today about BowelScreen Australia, or order a screening test online or by calling Bowel Cancer Australia's Helpline on 1800 727 336.
* People with (i) no first- or second-degree relative with bowel cancer; or (ii) one first-degree relative with bowel cancer diagnosed at 55 years or older; or (iii) one first-degree and one second-degree relative diagnosed with bowel cancer at 55 years or older.

Bowel cancer surveillance
People from families with bowel cancer need extra testing to find bowel cancer early. This could include having regular colonoscopies.
The age at which a person should start regular bowel check-ups depends on their risk category.
They may also be advised to start taking low-dose aspirin regularly from age 25.
If you think you have a family history of bowel cancer or an inherited gene mutation, you should make an appointment with your GP to talk about your own risk.
If a person experiences symptoms suggestive of bowel cancer for two weeks or longer, they should be referred by their GP to a specialist for colonoscopy within 30 days in order to investigate the cause.
Even if the person is not experiencing any symptoms suggestive of bowel cancer, if they receive a positive result from an at-home screening test, known as a faecal immunochemical test (FIT), they should be referred by their GP to a specialist for colonoscopy within 30 days for further investigation.
| What is a colonoscopy?
A colonoscopy is a detailed examination which looks at the lining of the entire large bowel.
During the procedure, if the colonoscopist sees anything that needs further investigation, photographs and samples (biopsies) can be taken and simple polyps can be removed.
| What is a CT scan?
Sometimes the first sign of bowel cancer is sudden blockage of the bowel.
When this happens, bowel cancer is diagnosed by computed tomography (CT scan) and an emergency operation.
Following a bowel cancer diagnosis, specialists determine how far cancer has spread. This process is called cancer staging.
There are several different systems for recording cancer stage.
All these systems use codes based on letters and numbers, to indicate the extent of cancer spread and how much cancer is still in the body after surgery.
Australian specialists use a combination of these systems.
Staging is done by a combination of colonoscopy and scans, such as CT, positron emission tomography (PET scan), and magnetic resonance imaging (MRI).
Pathology testing of the cancer sample is also conducted and involves looking at cancer under a microscope and testing for genetic changes in the cancer cells.
The pathologist works closely with the surgeon to get an accurate understanding of the individual’s cancer.
This testing can help identify the best treatment for the person.

How long an individual will live after a diagnosis of cancer (prognosis) is affected by a range of factors, such as the specific characteristics of the individual, including their age and general health at the time of diagnosis, the type and stage of cancer they have, and the treatments received.
The 5-year relative survival of 98.6% for people diagnosed with stage I bowel cancer means these people had a 9 in 10 chance surviving five years after diagnosis relative to comparable people in the general population.
Please note, 5-year relative survival does not reflect an individual's chance of surviving cancer.

Just as everyone is different, so is their bowel cancer treatment plan, which will be tailored to the patient’s individual circumstances.
Treatments can include surgery, chemotherapy, radiation or a combination of these.
Screening for loss of expression of mismatch repair protein (MMR) is recommended following surgery if you are under age 50.
Everyone diagnosed with bowel cancer age 70 or younger should have their tumour screened for Lynch syndrome to determine if they carry the genetic mutation.
If they do, they and their family members should receive a referral to a Specialist and a Family Cancer Clinic to discuss screening and surveillance.
| Follow-up after surgery
Patients with primary bowel cancer who have received treatment should be reviewed at 3-6 monthly intervals during the first year, 6 monthly for the next 2 years, and then annually for another 2 years (i.e. follow-up over a 5 year period in total at varying intervals).
Follow-up should include blood tests to measure levels of carcinoembryonic antigen (CEA), surveillance colonoscopies, CT scans, and PET or MRI scans if further investigation is required.
A novel blood test to detect bowel cancer recurrence has been developed by Australian scientists from CSIRO, Flinders University and Clinical Genomics (manufacturer and pathology service provider for the BowelScreen Australia program).
The 2-gene (BCAT1 and IKZF1) liquid biopsy targeting tumour DNA has been launched in the US but is not currently available in Australia. If successful, the test could replace the CEA monitoring regime currently being used.
| What if the cancer returns or spreads?
Risk for recurrence of bowel cancer is highest within the first five years after diagnosis. For those who have had bowel cancer previously no matter how long ago, there is a greater chance of developing new bowel cancers than for those without a history of the disease.
Following initial treatment, 30-50% of bowel cancer patients in remission develop recurrence, typically within the first 2 - 3 years following treatment. If it does, it may or may not cause symptoms, which is why surveillance is essential.
If the bowel cancer has spread (metastasised) throughout the body through the blood or lymph nodes, it will most likely affect the liver and lungs.
As with the original treatment plan, the approach taken will vary depending on the individual. RAS and BRAF testing is recommended as soon as you are diagnosed with advanced (metastatic) bowel cancer (mCRC).
RAS testing is important because it can give your oncologist information they need to decide if adding a targeted therapy (precision medicine) to your chemotherapy treatments may work for you.
Personalising (or tailoring) medical treatment according to your genetic make-up helps:
- avoid potential adverse effects from ineffective treatments
- avoid delay in seeking alternative treatments which may be effective
- reduce the costs of ineffective treatment.
For people with bowel cancer that is not curable by surgery, treatment aims to prolong survival and improve quality of life.
Bowel Cancer Australia provides practical and emotional support for the growing number of Australians affected by the disease.
The 100% community-funded charity offers information, resources, and support to anyone with issues related to bowel cancer.
To speak with a Bowel Care Nurse please call 1800 555 494 between 10am – 4pm, Monday to Friday, or email anytime.