| Sustainable funding to expand Australia's bowel cancer research capacity
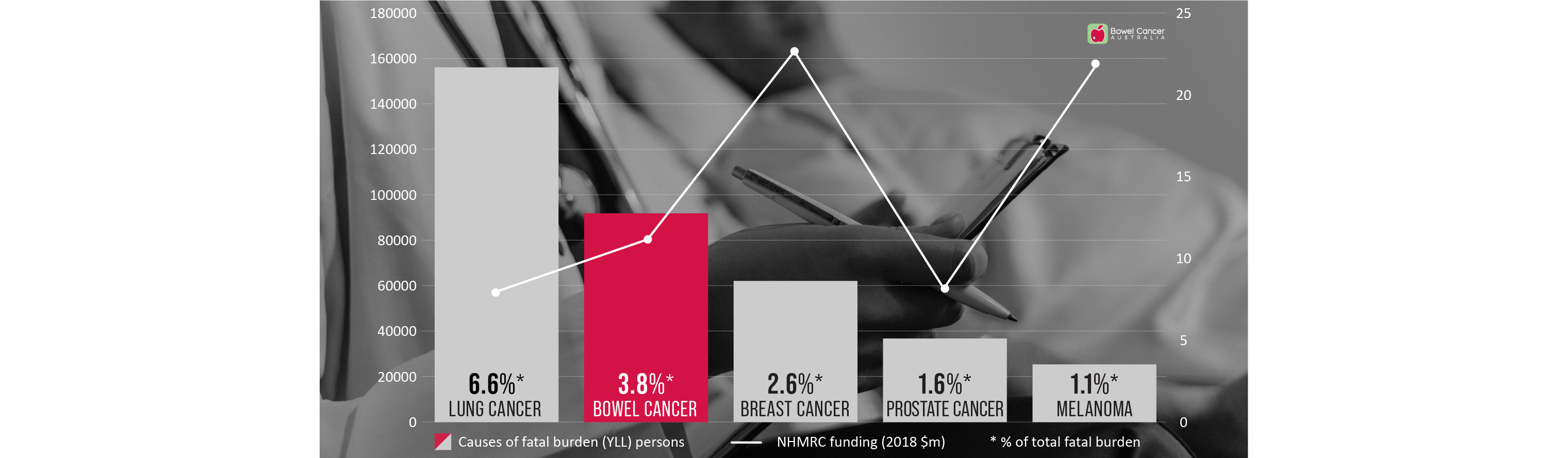
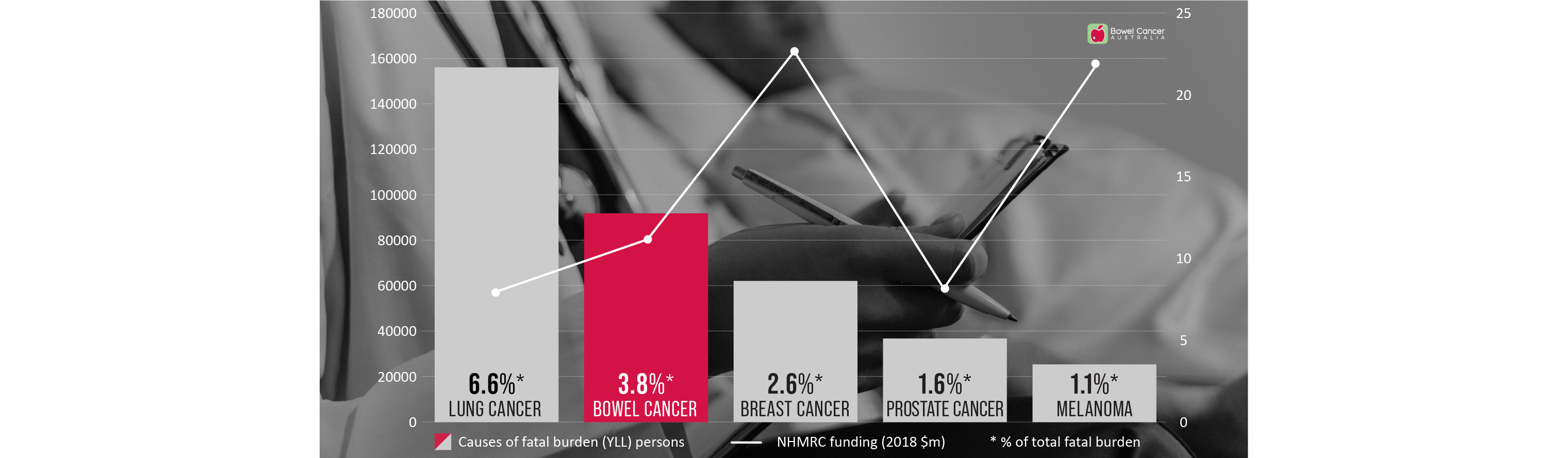
Bowel cancer is Australia's second deadliest cancer and has the second highest disease burden of any cancer in Australia.
Burden of disease measures the impact of living with illness and injury or dying prematurely.
However, bowel cancer received around 55 percent less research funding from the National Health and Medical Research Council (NHMRC) compared to breast cancer (2021: $8.6 million v $19.1 million); and receives no government funding to support dedicated Bowel Care Nurse Specialists, compared to $120 million for 98 Breast Care Nurse Specialists; $33 million for 62 Prostate Cancer Nurse Specialists, and $6.9 million for 5 Lung Cancer Nurse Specialists.
Burden of disease measures the impact of living with illness and injury or dying prematurely.
However, bowel cancer received around 55 percent less research funding from the National Health and Medical Research Council (NHMRC) compared to breast cancer (2021: $8.6 million v $19.1 million); and receives no government funding to support dedicated Bowel Care Nurse Specialists, compared to $120 million for 98 Breast Care Nurse Specialists; $33 million for 62 Prostate Cancer Nurse Specialists, and $6.9 million for 5 Lung Cancer Nurse Specialists.
To help address this research funding inequity, Bowel Cancer Australia established the Bowel Cancer Research Foundation Australia.
An objective of the Foundation is to support and sustainably fund research into the causes, prevention and treatment of bowel cancer to benefit us all in the future. While Bowel Cancer Australia is here today supporting, informing and caring for people affected by the disease.
Through the Foundation, Bowel Cancer Australia has made a significant investment in the Lawrence Penn Chair of Bowel Cancer Research, dedicated to leading edge bowel cancer discoveries that aim to have an everlasting impact on Australia's health future.
The establishment of the Lawrence Penn Chair, in collaboration with the University of Sydney and the Kolling Institute, strengthens our collective pursuit of a bowel cancer cure.
Other major bowel cancer projects funded to date, include the ASCOLT Clinical Trial; ICHOM Colorectal Cancer Standard Set; patient-reported experiences (My Colonoscopy Experience), community awareness and understanding; patient and metastatic patient lived-experiences; and demographic research.
To date, Bowel Cancer Australia, collaboratively with funding partners, has funded over $12.5 million in bowel cancer research projects.
You can make a lasting contribution to bowel cancer research through a donation or a bequest (a gift made in your Will) to Bowel Cancer Australia or by calling us on 1800 727 336.

Through the Foundation, Bowel Cancer Australia has made a significant investment in the Lawrence Penn Chair of Bowel Cancer Research, dedicated to leading edge bowel cancer discoveries that aim to have an everlasting impact on Australia's health future.
The establishment of the Lawrence Penn Chair, in collaboration with the University of Sydney and the Kolling Institute, strengthens our collective pursuit of a bowel cancer cure.
Other major bowel cancer projects funded to date, include the ASCOLT Clinical Trial; ICHOM Colorectal Cancer Standard Set; patient-reported experiences (My Colonoscopy Experience), community awareness and understanding; patient and metastatic patient lived-experiences; and demographic research.
To date, Bowel Cancer Australia, collaboratively with funding partners, has funded over $12.5 million in bowel cancer research projects.
You can make a lasting contribution to bowel cancer research through a donation or a bequest (a gift made in your Will) to Bowel Cancer Australia or by calling us on 1800 727 336.

| Researching improved follow-up colonoscopy surveillance timings
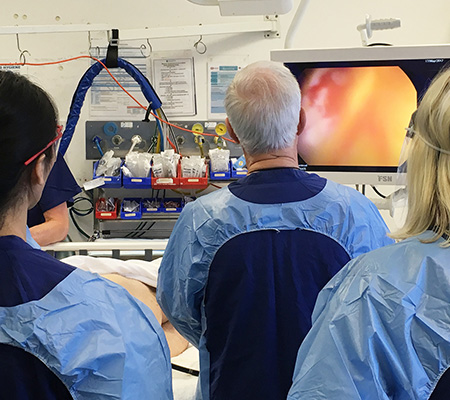
Profiling of 60 bowel adenoma polyps will be used to better define optimal colonoscopic surveillance intervals, thanks to a new research grant to the Lawrence Penn Chair of Bowel Cancer Research from the Medical Research Future Fund (Sydney Health Partners).
Professor Mark Molloy, and his collaborators including Professor Alexander Engel from Royal North Shore Hospital will use molecular analysis of bowel polyps to investigate disease risk, seeking to find a signature of transformation risk which could potentially be used to optimise colonoscopy surveillance intervals.
"The research grant provided by the Medical Research Future Fund is exciting as it allows us to trial a pathway for molecular testing of bowel polyps and see if this information can tell us more about a given patient's bowel cancer risk,” said Professor Mark Molloy.
“It may offer an opportunity for more personalised prognosis as we will consider genetic, proteomic and microbiome features of these precancerous growths, which are not currently part of routine pathology testing," he added.
Researchers will use the local health district colonoscopy screening clinic to collect and analyse up to 60 polyps of varying risk levels.
"We will also explore if this molecular information may be useful for guiding follow-up colonoscopy surveillance timing as this would help improve scheduling and costs," Professor Molloy said.

| Researching why some early stage bowel tumours metastasise to lymph nodes
Funding from the Colorectal Surgical Society ANZ Foundation will support new research to improve our understanding of why some early stage bowel tumours metastasise to lymph nodes.
“This is important because patients with lymph node disease have worse prognosis and face more intense treatment than patients whose cancer remains within the bowel wall,” said Lawrence Penn Chair of Bowel Cancer Research Professor Mark Molloy.
The $60,000 research grant awarded to the Chair will enable molecular analysis to refine risk of dissemination in early stage tumours and transformation potential of some bowel polyps.
“Patients with Stage I bowel cancer have a greater than 98% 5-year rate of survival which falls to around 70% when the tumour has metastasized to lymph nodes,” Professor Molloy said.
“We need to better understand this process to develop medical interventions and stop the tumour disseminating elsewhere," he added.
The project will generate preliminary data using genomic sequencing of early stage tumours and malignant bowel polyps. Professor Molloy and his team aim to link these mutations with those early tumours which spread to lymph nodes, providing a biomarker of risk which may inform surgical pathways.
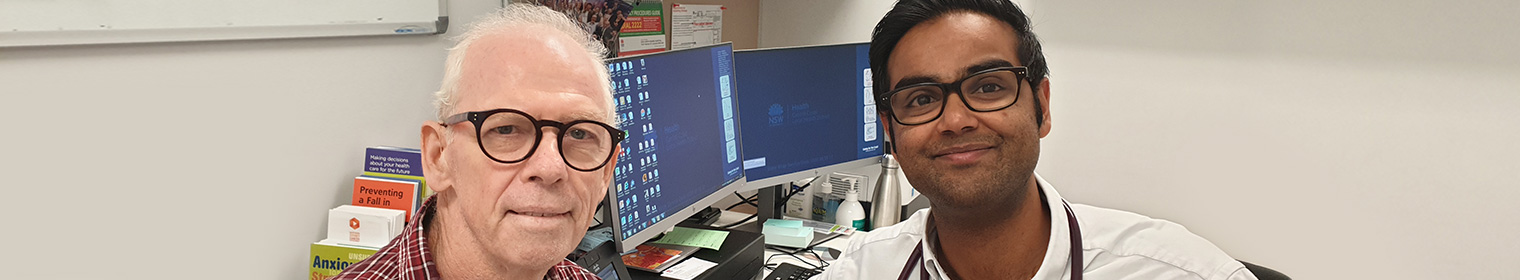
| Dr Mudy De Silva awarded the Penelope Morris Foundation Scholarship
Dr Mudy De Silva is a Medical Oncologist with a special interest in clinical trials and translational research in gastrointestinal cancers.
While doing clinical training Medical Oncology at Royal North Shore Hospital in Sydney, he developed a strong interest in bowel cancer.
“What I find interesting and challenging about bowel cancer research is the complex interplay of tumour, genes, gut microbiome, and the immune system,” said Mudy.
Mudy is also curious as to why immunotherapies, which have led to landmark survival rates in several other cancers, do not appear to be effective for most patients with bowel cancer.
“Furthermore, there is an alarming trend indicating young onset bowel cancers are on the rise,” said Mudy.
“Personally, I have come across many younger patients with bowel cancer at various stages, including two young women who were diagnosed with metastatic disease during pregnancy.”
“These latter cases have impressed upon me the need to understand more about the biology, behaviour, and management of bowel malignancies.”
As the recipient of the highly coveted Penelope Morris Foundation PhD scholarship offered through The University of Sydney, Mudy will be able to focus his studies on the molecular analysis of young onset bowel cancer under the supervision of Lawrence Penn Chair Professor Mark Molloy and eminent medical oncologist, Professor Stephen Clarke.
“It is an absolute pleasure to be involved with translation research in bowel cancer, and I am deeply grateful to Professor Mark Molloy as well as the Penelope Morris Foundation for facilitating this work,” Mudy said.
“I sincerely hope to bring discoveries from our lab to the clinic and translating them into clinically meaningful benefits for patients.”
“Despite significant improvements over the past 4 to 5 decades, the 5-year overall survival of patients with metastatic disease remains poor at around 15%.”
“Furthermore, data from registries of real-world patients suggest there has been no improvement in overall survival for patients with metastatic disease since 2008.”
“At present, we give empirical therapies to patients with bowel cancer based on just a few biomarkers, highlighting the significant need for discovery of novel biomarkers and therapeutic strategies through translational research,” said Mudy.
“We now have a better understanding that the clinical activity of many cancer therapies can be attributed to the re-establishment of immune surveillance within the tumour microenvironment through a specific type of immunogenic cell death (ICD).”
“ICD is unique to other forms of regulated cell death and necrosis in that it produces a robust anti-tumour adaptive immune response, which can be lasting.”
“There are several hallmarks of ICD, and I am keen to explore whether these are detectable with currently available technologies, and whether they have prognostic or predictive value as biomarkers.”
Mudy will also be exploring which treatment strategies optimise immunogenic cell death, in order to better understand how cancers develop resistance to it.

| Dr Zoe Welham awarded The Penn Foundation Scholarship
Zoe developed an interest in bowel cancer while she was working on a complex scientific research project in graduate school.
“The goal was to look at bowel cancer in a holistic way by taking information from genes, microbes and epigenetic data,” Zoe said.
As a PhD recipient of The Penn Foundation Scholarship at The University of Sydney, Zoe will now be able to build on that analysis under the supervision of the Lawrence Penn Chair of Bowel Cancer Research, Professor Mark Molloy.
Zoe will compare the microbiomes of polyps at different risk levels for developing bowel cancer, to better understand how the gut microbiome influences the growth of bowel polyps.
She will also investigate the metabolites these microbes produce (such as butyrate, which is thought to be an important energy source for colon epithelia), to see how they correlate with polyp risk.
She will then study ways to integrate this data with other molecular features and with the patient’s medical history.
Through her research, Zoe aims to provide valuable new knowledge regarding the biological rules that govern bowel polyp growth – something which is still not fully understood.
“The gut microbiome is interesting because of how it appears to play a role in a wide range of health issues, from food metabolism, to interacting with our immune system, and even influencing neurological traits,” said Zoe.
“Humans enjoy a symbiotic relationship with our bugs."
“We provide food and they help with food digestion and provide molecules that influence many of our body processes."
“I also find it interesting that, unlike our genes, we can control what bugs make up our microbiomes to some an extent – simply by changing our diets."
“For example, research suggests that people with high meat intake have different ratios of gut bacteria to people who eat less meat."
“This is interesting, given excess red meat consumption is a risk factor for bowel cancer.”
Zoe hopes her work will ultimately lead to a reduction in bowel cancer.
Benita is a junior post-doctoral fellow and Immunologist who is helping identify new ways to regulate polyp development through microscopy assays that phenotype the different immune cells in polyps and surrounding mucosa.
| Dr Pascal Steffen awarded Early Career Fellowship
A new grant secured by the Lawrence Penn Chair of Bowel Cancer Research laboratory from the Cancer Institute NSW will enable further investigation into the prognostic contribution of immune cell infiltration in rectal cancer.
The $600,000 grant will provide a three-year fellowship salary for Dr Pascal Steffen and help to cover some research costs for him to apply proteomic techniques to investigate the role of immune cells in rectal cancer.
Approximately 5,000 Australian men and women are diagnosed with rectal cancer each year. The aim of Dr Steffen’s CINSW fellowship is to understand the involvement of immune cell infiltration in rectal cancer, how this impacts tumour biology and how it affects patient outcomes.
To conduct the study over the next three years, Dr Steffen will apply his knowledge of protein mass spectrometry with access to the large archival rectal cancer tissue database at Royal North Shore Hospital. He will map the proteome (proteins found in the cancer) of these rectal cancers to understand their biology and how this links to patient prognosis, and work to resolve the complex immune cell architecture of these cancers by using a new technique of imaging mass cytometry.
The outcome of this research will lead to new prognostic biomarker panels, provide a better understanding of immune cells in rectal cancers and pave the way for new treatments.
“I am very excited to receive the CINSW fellowship as it will allow me to apply my expertise in proteomics to the cause of advancing the understanding of the role of immune cells in rectal cancer and furthering the research of new ways to combat this disease. This fellowship will also grant me the opportunity to broaden my knowledge especially in the field of immunology and imaging techniques,” said Dr Steffen.
Dr Pascal Steffen will conduct his fellowship in the Bowel Cancer and Biomarker Laboratory at The Kolling Institute, Royal North Shore Hospital in Sydney under the supervision of Professor Mark Molloy, Lawrence Penn Chair of Bowel Cancer Research, The University of Sydney.
“One of the key objectives for the Chair of Bowel Cancer Research is to increase research capacity and foster researcher development. I am delighted that the CINSW is supporting our vision through the award of this prestigious fellowship to Pascal. His research will reveal important new understandings in rectal cancer which is an essential step towards improving the outcomes for people with this disease,” Professor Molloy said.
Dr Pascal Steffen is a post-doctoral research associate (early career research fellow) and the newest member of the team working with the Lawrence Penn Chair of Bowel Cancer Research, Professor Mark Molloy.
The $600,000 grant will provide a three-year fellowship salary for Dr Pascal Steffen and help to cover some research costs for him to apply proteomic techniques to investigate the role of immune cells in rectal cancer.
Approximately 5,000 Australian men and women are diagnosed with rectal cancer each year. The aim of Dr Steffen’s CINSW fellowship is to understand the involvement of immune cell infiltration in rectal cancer, how this impacts tumour biology and how it affects patient outcomes.
To conduct the study over the next three years, Dr Steffen will apply his knowledge of protein mass spectrometry with access to the large archival rectal cancer tissue database at Royal North Shore Hospital. He will map the proteome (proteins found in the cancer) of these rectal cancers to understand their biology and how this links to patient prognosis, and work to resolve the complex immune cell architecture of these cancers by using a new technique of imaging mass cytometry.
The outcome of this research will lead to new prognostic biomarker panels, provide a better understanding of immune cells in rectal cancers and pave the way for new treatments.
“I am very excited to receive the CINSW fellowship as it will allow me to apply my expertise in proteomics to the cause of advancing the understanding of the role of immune cells in rectal cancer and furthering the research of new ways to combat this disease. This fellowship will also grant me the opportunity to broaden my knowledge especially in the field of immunology and imaging techniques,” said Dr Steffen.
Dr Pascal Steffen will conduct his fellowship in the Bowel Cancer and Biomarker Laboratory at The Kolling Institute, Royal North Shore Hospital in Sydney under the supervision of Professor Mark Molloy, Lawrence Penn Chair of Bowel Cancer Research, The University of Sydney.
“One of the key objectives for the Chair of Bowel Cancer Research is to increase research capacity and foster researcher development. I am delighted that the CINSW is supporting our vision through the award of this prestigious fellowship to Pascal. His research will reveal important new understandings in rectal cancer which is an essential step towards improving the outcomes for people with this disease,” Professor Molloy said.
Dr Pascal Steffen is a post-doctoral research associate (early career research fellow) and the newest member of the team working with the Lawrence Penn Chair of Bowel Cancer Research, Professor Mark Molloy.
| Mass spectrometry core facility opens
Professor Molloy’s focus is on molecular analysis, which can improve understanding of tumour biology and help clinicians make decisions about treatment. It is an area of research that could have a profound impact on the care of bowel cancer patients.
“There is no doubt that technology is driving a big revolution in clinical care,” Professor Molloy said.
One example of this technological transformation is the use of mass spectrometers – sophisticated weighing devices that allow researchers to determine the molecular make-up of various substances.
With two new mass spectrometers installed at the Kolling Institute, Professor Molloy and his team will analyse the molecular features of proteins and metabolites in individual tumours, to tailor treatment pathways according to the needs of each patient.
"When combined with genomic analysis, this gives us a more complete molecular picture of bowel cancer, which is essential to better understand prevention and treatment strategies," Professor Molloy said.
Mass spectrometers could also be used to monitor medication levels in a patient’s body, allowing clinicians to deliver a dose precisely calibrated to suit the individual patient.
The goal is to find ways of integrating molecular analysis into everyday patient care. Professor Molloy envisages that within the next five years clinical teams working with bowel cancer patients could include a molecular scientist.
“Today, these multidisciplinary teams discuss imaging, surgery, approaches to chemotherapy and so on,” he said.
“I’d like to see clinicians also asking how molecular analysis could help add to the fuller picture.”
At the opening of the new facility earlier this month, Professor Molloy explained how the two state-of-the-art mass spectrometry instruments would underpin his research team's effort to map the proteome (the proteins) and metabolome (the metabolites) from specimens provided by bowel cancer patients.
The facility was made possible with a significant financial gift of $500,000 from Bowel Cancer Australia and the Bowel Cancer Research Foundation Australia.
“These new mass spectrometers will have a profound impact on the future of patient treatment and care by allowing researchers to more closely examine bowel polyps, precancerous growths that can grow into cancers, to better understand why they develop in some people,” said Professor Molloy.
Professor Molloy demonstrated how the mass spectrometer can map the proteome using a very small amount of bowel cancer on a pathology slide, revealing the instrument’s incredible capabilities in providing biological information compared to older systems.
“This is viewed as a key aspect of understanding the triggers that allow bowel cancers to grow and metastasize to other body locations,” he added.
Research undertaken by the Lawrence Penn Chair of Bowel Cancer Research is aiming to give new information to clinicians that will better inform them of appropriate treatment pathways based on the molecular information encoded in a patient’s polyp or tumour.
The Lawrence Penn Chair continues to emphasise the importance of research to understand ways we can prevent bowel cancer and to lead the way in providing better treatments for bowel cancer patients.