There are different types of treatment for patients with bowel cancer, depending on where the cancer is located in the body (i.e. the colon or rectum).
While surgery is the most common treatment for removing the cancer from your bowel, some people may also require chemotherapy and/or radiotherapy to reduce the size of the tumour and prevent progression of the disease.
If surgery is not an option, then chemotherapy and radiotherapy may be offered to halt progression of the disease and to help control the symptoms.
Treatment for bowel cancer is decided by:
- Where the cancer is in your bowel
- How big the tumour is
- The number, size and position of any tumours outside the bowel (including lymph nodes)
- The type of cancer cells – their cell type and genetic makeup
- Your general health and fitness
- Your wishes as the patient
It will also be determined by:
- Medical guidelines for best practice in treating bowel cancer
- The availability of different treatment options within your local hospital
- The access to clinical trials available within your local hospital
- How well you respond to the treatments
- The impact of any side-effects you may experience as a result of treatment
- What kind of operation do you recommend for me?
- Do I need any lymph nodes removed?
- Will other tissues be removed?
- Why?
- What are the risks of surgery?
- Will I have any lasting side effects?
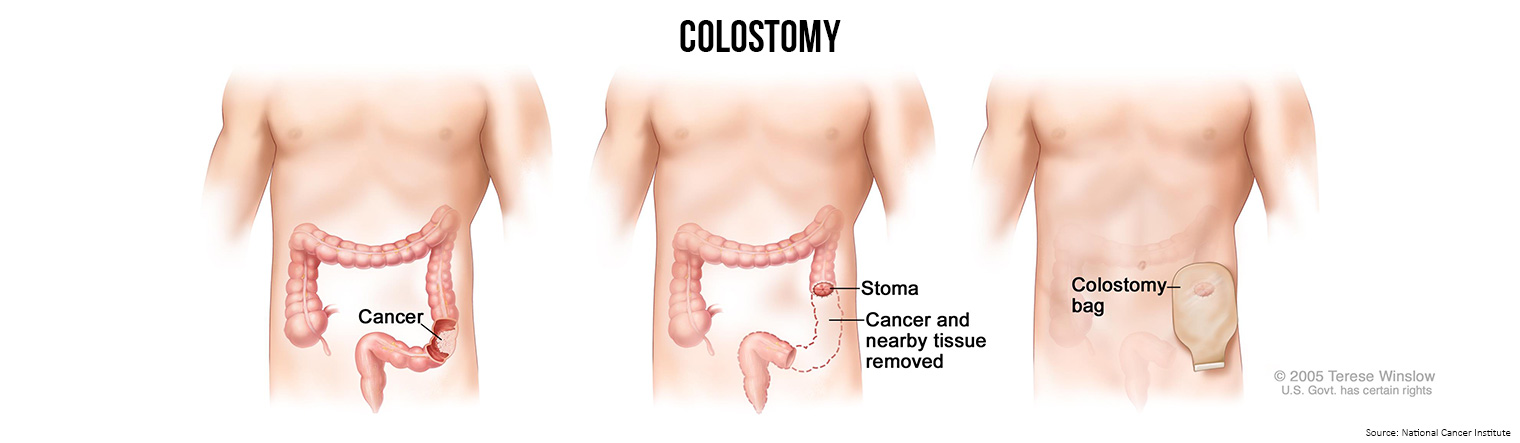
- Will I need a colostomy?
- If so, will the stoma be permanent?
- How will I feel after the operation?
- If I have pain, how will it be controlled?
- How long will I be in the hospital?
- When can I get back to my normal activities?
It is common to feel tired or weak for a while. Also, surgery sometimes causes constipation or diarrhoea. Your health care team monitors you for signs of bleeding, infection, or other problems requiring immediate treatment.
There are seven types of standard treatment for patients with colon cancer.
- Local excision: If the cancer is found at a very early stage, the surgeon may remove it without cutting through the abdominal wall. Instead, the surgeon may put a tube with a cutting tool through the rectum into the colon and cut the cancer out. This is called a local excision. If the cancer is found in a polyp, the operation is called a polypectomy.
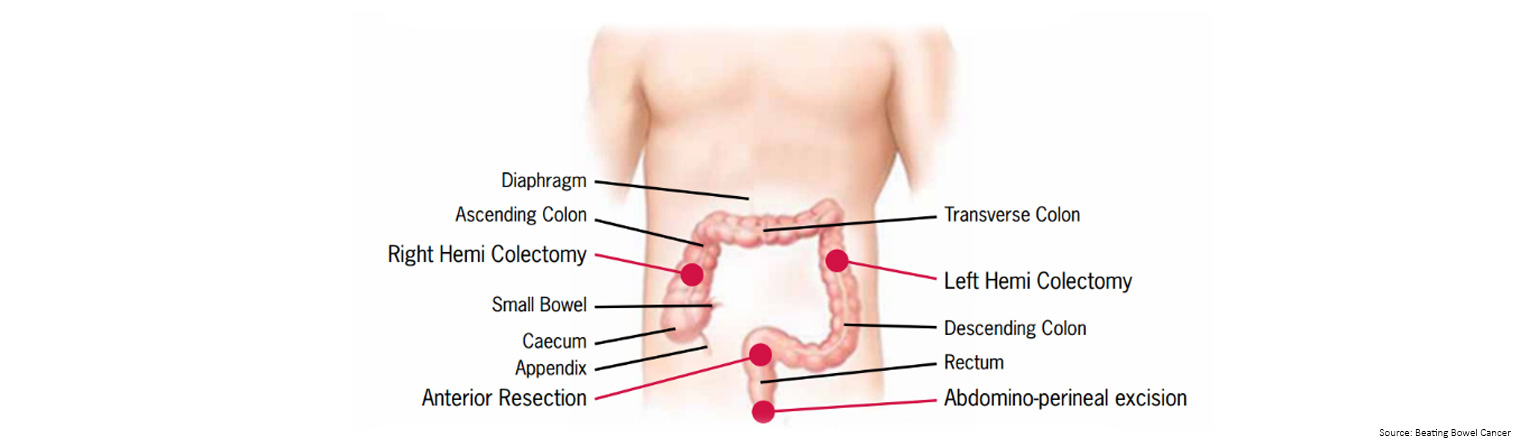
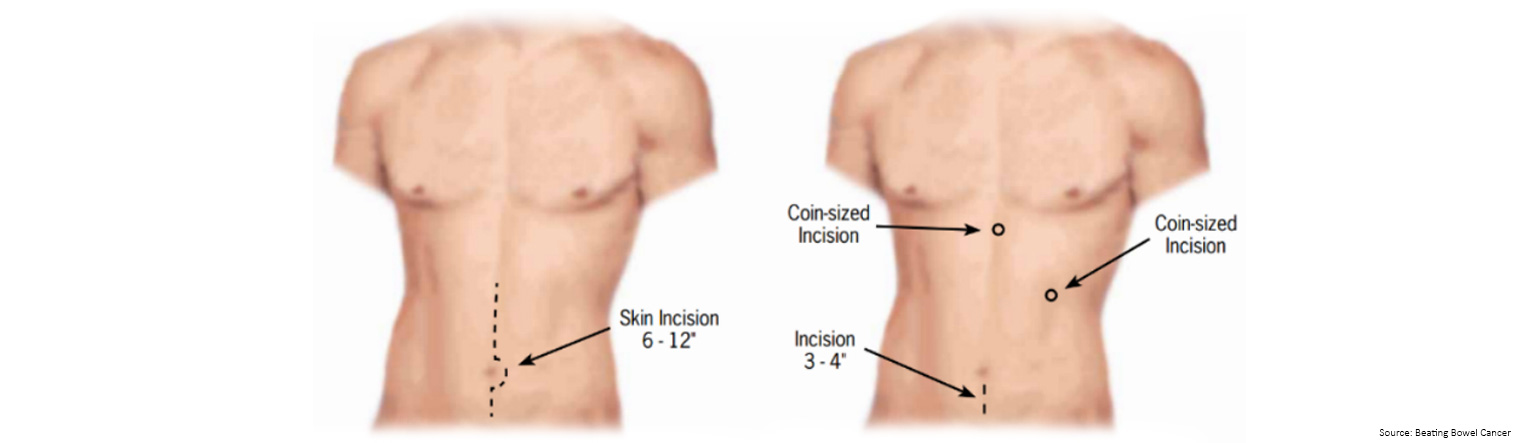
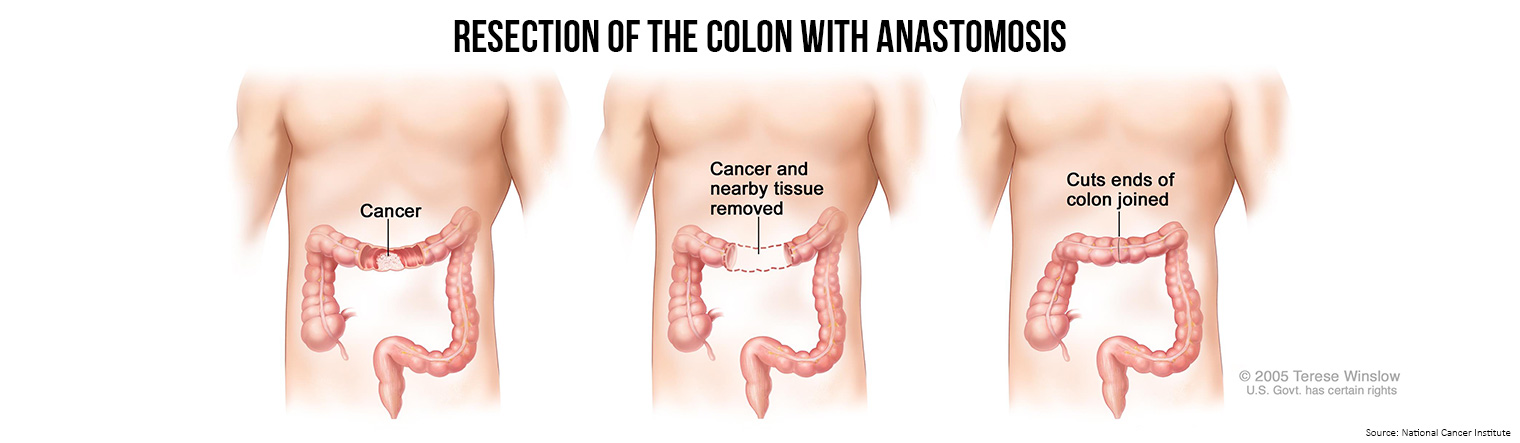
- Resection of the colon with anastomosis: If the cancer is larger, the surgeon will perform a partial colectomy (removing the cancer and a small amount of healthy tissue around it). The surgeon may then perform an anastomosis (sewing the healthy parts of the colon together). The surgeon will also usually remove lymph nodes near the colon and have them examined under a microscope to see whether they contain cancer.
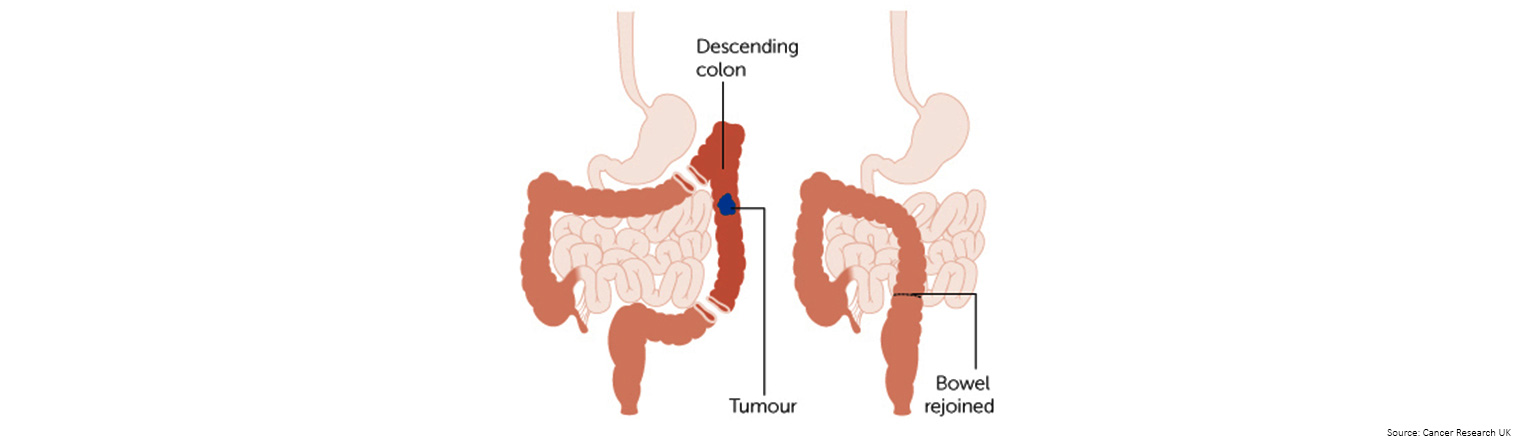 If the left side of the colon is removed, the operation is called a left hemi colectomy
If the left side of the colon is removed, the operation is called a left hemi colectomy
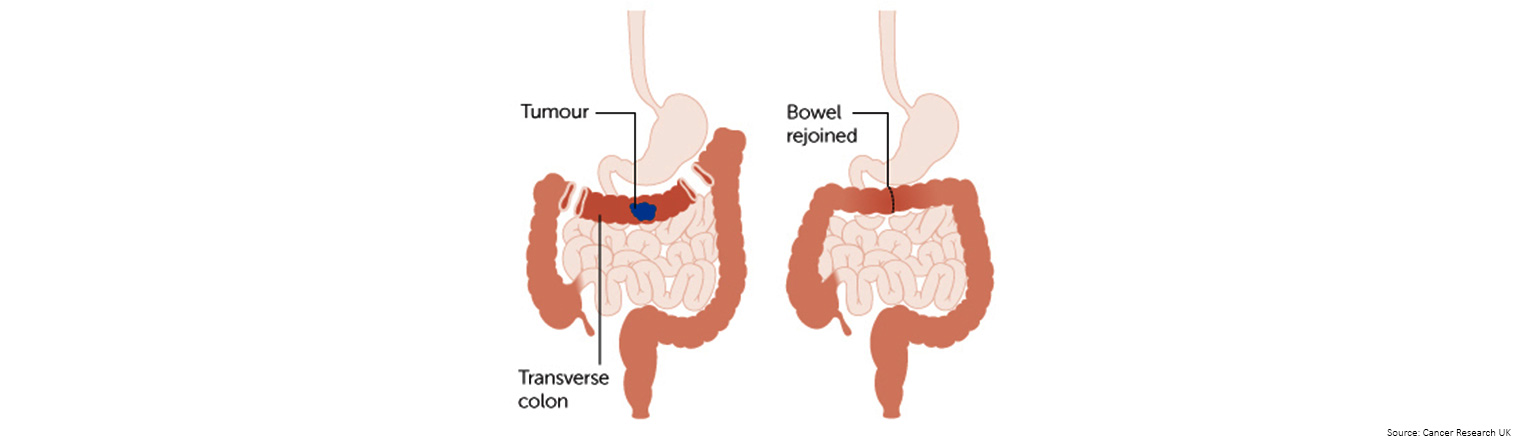 If the middle part of the bowel is removed the transverse colon) it is called a transverse colectomy
If the middle part of the bowel is removed the transverse colon) it is called a transverse colectomy
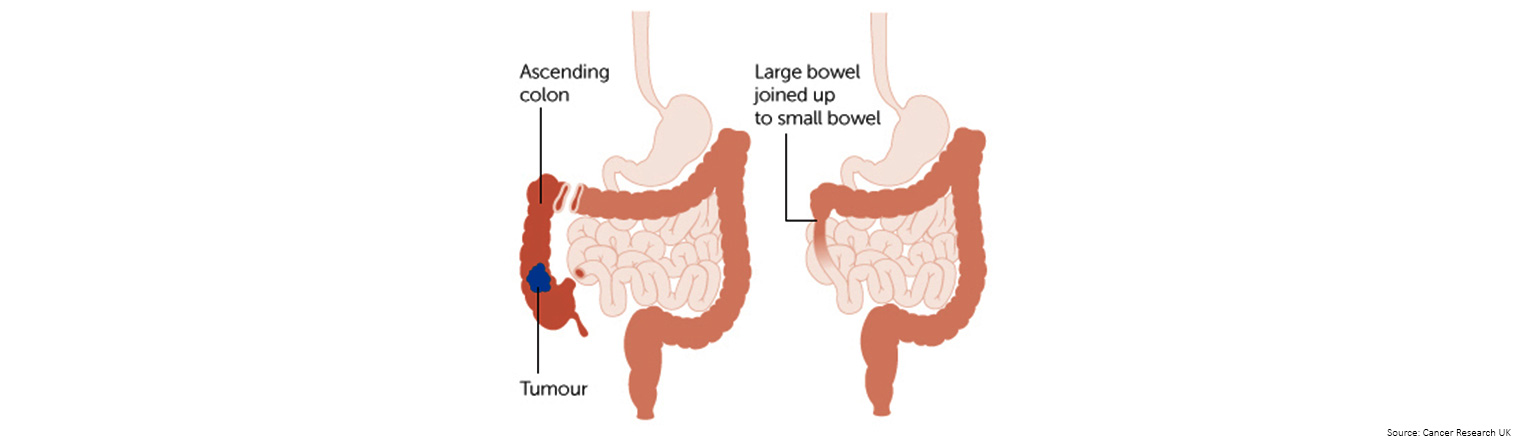 If the right side of the colon is removed, it is called a right hemicolectomy
If the right side of the colon is removed, it is called a right hemicolectomy
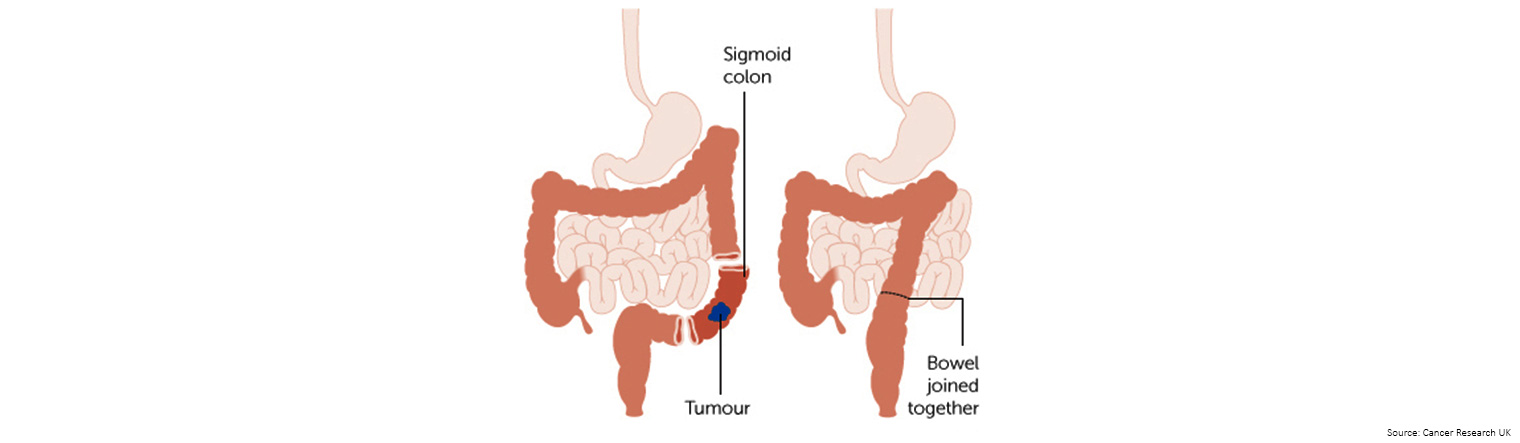 If the sigmoid colon is removed it is called a sigmoid colectomy
If the sigmoid colon is removed it is called a sigmoid colectomy
- Resection of the colon with colostomy: If the surgeon is not able to sew the two ends of the colon back together, a stoma (an opening) is made on the outside of the body for waste to pass through. This procedure is called a colostomy. A bag is placed around the stoma to collect the waste. Sometimes the colostomy is needed only until the lower colon has healed, and then it can be reversed. If the surgone needs to remove the entire lower colon, however, the colostomy may be permanent.
After the surgeon removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Radiofrequency ablation
Cryosurgery
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping the cells from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly in the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
Chemoembolisation of the hepatic artery is a type of regional chemotherapy that may be used to treat cancer that has spread to the liver. This is done by blocking the hepatic artery (the main artery that supplies blood to the liver) and injecting anticancer drugs between the blockage and the liver. The liver’s arteries then carry the drugs into the liver. Only a small amount of the drug reaches other parts of the body. The blockage may be temporary or permanent, depending on what is used to block the artery. The liver continues to receive some blood from the hepatic portal vein, which carries blood from the stomach and intestine.
The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Radiation Therapy
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. Types of targeted therapies used in the treatment of colon cancer include monoclonal antibodies and angiogenesis inhibitors.
Immunotherapy
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are taking place in many parts of Australia and around the world, visit Bowel Cancer Australia's clinical and treatment Trials webpage for more information.

- Local excision or simple polypectomy.
- Resection and anastomosis. This is done when the tumor is too large to remove by local excision.
Stage I colon cancer
- Resection and anastomosis.
- Resection and anastomosis.
- Resection and anastomosis which may be followed by chemotherapy.
- Clinical trials of new chemotherapy regimens after surgery.
- Local excision for tumors that have recurred.
- Resection with or without anastomosis.
- Surgery to remove parts of other organs, such as the liver, lungs, and ovaries, where the cancer may have recurred or spread. Treatment of cancer that has spread to the liver may also include the following:
- Chemotherapy given before surgery to shrink the tumor, after surgery, or both before and after.
- Radiofrequency ablation or cryosurgery, for patients who cannot have surgery.
- Chemoembolisation of the hepatic artery.
- Radiation therapy or chemotherapy may be offered to some patients as palliative therapy to relieve symptoms and improve quality of life.
- Chemotherapy and/or targeted therapy with a monoclonal antibody or an angiogenesis inhibitor.
- Immunotherapy.
- Clinical trials of chemotherapy and/or targeted therapy.
Surgery
- Polypectomy: If the cancer is found in a polyp (a small piece of bulging tissue), the polyp is often removed during a colonoscopy.
- Local excision: If the cancer is found on the inside surface of the rectum and has not spread into the wall of the rectum, the cancer and a small amount of surrounding healthy tissue is removed.
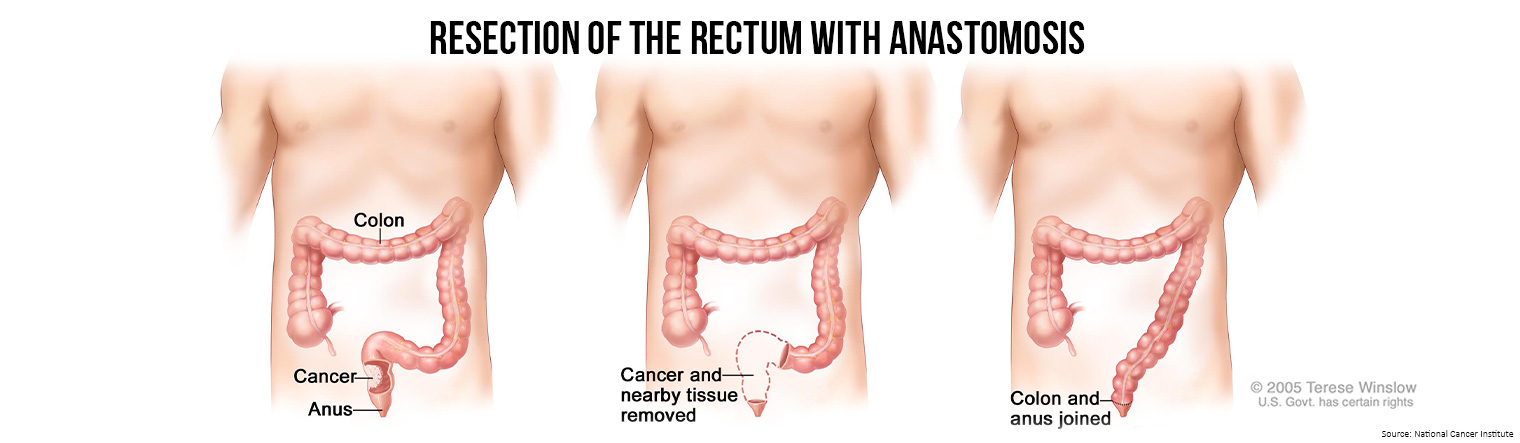
- Resection: If the cancer has spread into the wall of the rectum, the section of the rectum with cancer and nearby healthy tissue is removed. Sometimes the tissue between the rectum and the abdominal wall is also removed. The lymph nodes near the rectum are removed and checked under a microscope for signs of cancer.
- Radiofrequency ablation: The use of a special probe with tiny electrodes that kill cancer cells. Sometimes the probe is inserted directly through the skin and only local anesthesia is needed. In other cases, the probe is inserted through an incision in the abdomen. This is done in the hospital with general anesthesia.
- Cryosurgery: A treatment that uses an instrument to freeze and destroy abnormal tissue. This type of treatment is also called cryotherapy.
- Pelvic exenteration: If the cancer has spread to other organs near the rectum, the lower colon, rectum, and bladder are removed. In women, the cervix, vagina, ovaries, and nearby lymph nodes may be removed. In men, the prostate may be removed. Artificial openings (stoma) are made for urine and stool to flow from the body to a collection bag.
After the cancer is removed, the surgeon will either:
- do an anastomosis (sew the healthy parts of the rectum together, sew the remaining rectum to the colon, or sew the colon to the anus);
- make a stoma (an opening) from the rectum to the outside of the body for poo to pass through. This procedure is done if the cancer is too close to the anus and is called a colostomy. A bag is placed around the stoma to collect the waste. Sometimes the colostomy is needed only until the rectum has healed, and then it can be reversed. If the entire rectum is removed, however, the colostomy may be permanent.
Radiation therapy and/or chemotherapy may be given before surgery to shrink the tumor, make it easier to remove the cancer, and help with bowel control after surgery. Treatment given before surgery is called neoadjuvant therapy. After all the cancer that can be seen at the time of the surgery is removed, some patients may be given radiation therapy and/or chemotherapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Radiation therapy
- External radiation therapy uses a machine outside the body to send radiation toward the cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
The way the radiation therapy is given depends on the type and stage of the cancer being treated. External radiation therapy is used to treat rectal cancer.
Short-course preoperative radiation therapy is used in some types of rectal cancer. This treatment uses fewer and lower doses of radiation than standard treatment, followed by surgery several days after the last dose.
Active surveillance
Active surveillance is closely following a patient's condition without giving any treatment unless there are changes in test results. It is used to find early signs that the condition is getting worse. In active surveillance, patients are given certain exams and tests to check if the cancer is growing. When the cancer begins to grow, treatment is given to cure the cancer. Tests include the following:
- Digital rectal exam
- MRI
- Endoscopy
- Sigmoidoscopy
- CT scan
- Carcinoembryonic antigen (CEA) assay
Targeted therapy
Immunotherapy
Stage 0 (Carcinoma in Situ)
Treatment of stage 0 may include the following:
- Simple polypectomy.
- Local excision.
- Resection (when the tumor is too large to remove by local excision).
Stage I Rectal Cancer
Treatment of stage I rectal cancer may include the following:
- Local excision.
- Resection.
- Resection with radiation therapy and chemotherapy after surgery.
Stages II and III Rectal Cancer
Treatment of stage II and stage III rectal cancer may include the following:
- Surgery.
- Chemotherapy combined with radiation therapy, followed by surgery.
- Short-course radiation therapy followed by surgery and chemotherapy.
- Resection followed by chemotherapy combined with radiation therapy.
- Chemotherapy combined with radiation therapy, followed by active surveillance. Surgery may be done if the cancer recurs (comes back).
- A clinical trial of a new treatment.
Stage IV and recurrent rectal cancer
Treatment of stage IV and recurrent rectal cancer may include the following:
- Surgery with or without chemotherapy or radiation therapy.
- Systemic chemotherapy with or without targeted therapy (angiogenesis inhibitor).
- Systemic chemotherapy with or without immunotherapy (immune checkpoint inhibitor therapy).
- Chemotherapy to control the growth of the tumor.
- Radiation therapy, chemotherapy, or a combination of both, as palliative therapy to relieve symptoms and improve the quality of life.
- Placement of a stent to help keep the rectum open if it is partly blocked by the tumor, as palliative therapy to relieve symptoms and improve the quality of life.
- Immunotherapy.
- Clinical trials of chemotherapy and/or targeted therapy.
Treatment of rectal cancer that has spread to other organs depends on where the cancer has spread.
- Treatment for areas of cancer that have spread to the liver includes the following:
- Surgery to remove the tumor. Chemotherapy may be given before surgery, to shrink the tumor.
- Cryosurgery or radiofrequency ablation.
- Chemoembolisation and/or systemic chemotherapy.
- A clinical trial of chemoembolization combined with radiation therapy to the tumors in the liver.
Anal cancer is a rare disease and treatment is quite specialised.
Please see our Bowel Cancer Australia's anal cancer webpage for more information.