A colonoscopy is a quick and generally painless procedure that allows for the full examination of the entire inner lining of your bowel (colon and rectum).
During the procedure, the colonoscopist spends most of the time looking for changes to the normal landscape of your bowel lining and removes anything that looks suspicious, like growths called polyps.
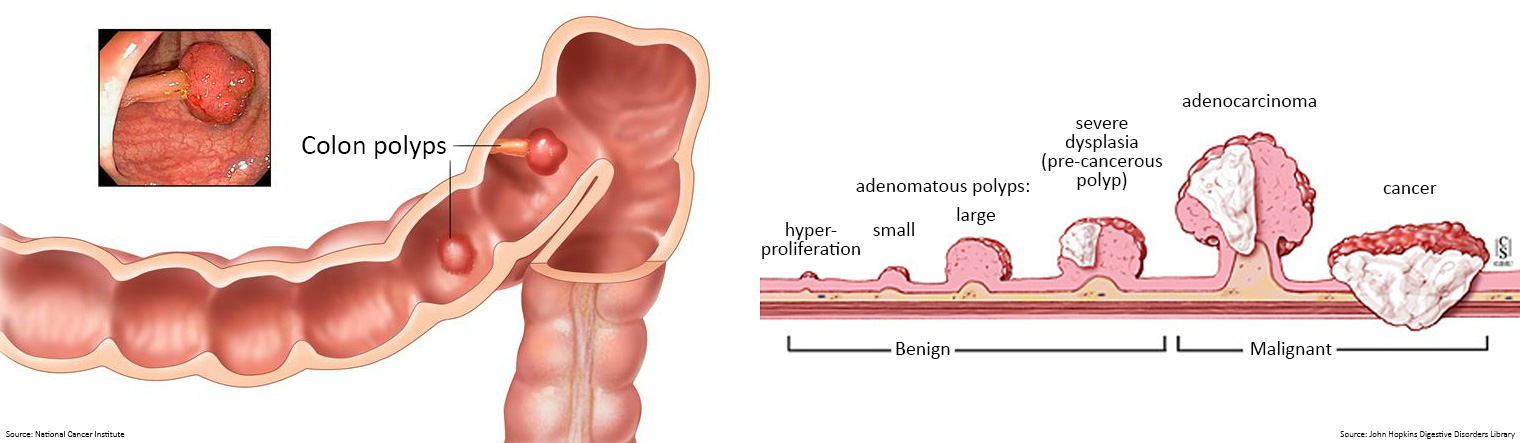
Polyps are usually harmless (benign); they can be slightly raised (sessile), look like they are on a stalk like a cherry (pedunculated), or can be very flat.
Adenomatous polyps however, can become cancerous (malignant), and if left undetected can develop into a cancerous tumour.
Polyps can be detected and removed before they develop into bowel cancer during a colonoscopy, and bowel cancer, if present, can be diagnosed.
The colonoscopy usually lasts around 30 minutes or less and is typically performed while you are under a general anaesthetic.
Because of the sedation, you should arrange for someone to collect you and take you home following the procedure.
| Why is the quality of colonoscopy important?
High quality colonoscopy is critical to the early detection and treatment of bowel cancer.
Removal of polyps and adenomas may prevent bowel cancer developing, while early diagnosis of bowel cancer can improve treatment outcomes and survival.
Colonoscopy can also identify those who require regular colonoscopy surveillance due to having an increased risk of bowel cancer.
The quality of colonoscopy is therefore important for minimising the risk of complications from the procedure.
Complications associated with colonoscopy include:
- risks of the procedure itself such as perforation and bleeding
- risks associated with bowel preparation including dehydration and electrolyte imbalances which can be serious
- complications arising from sedation or anaesthesia.
The risk of serious complications is approximately 4 perforations and 8 major bleeding events per 10,000 screening colonoscopies with an estimated mortality rate of 0.007%.
Risk increases with age, with the number of colonoscopies and when polyps are removed.
While the risk of complication is relatively small, a large number of people undergo colonoscopy, many of whom are not diagnosed with any disease.
| Why do I need a colonoscopy?
A colonoscopy is one of the most comprehensive methods to evaluate abnormalities within the bowel, including cancer, inflammation, bleeding, polyps, and adenomas, which are the precursor to bowel cancer.
A diagnostic colonoscopy is recommended if you experience symptoms suggestive of bowel cancer for two weeks or more, or if you receive a positive faecal immunochemical test (FIT) result.
If you have a genetic predisposition which increases your bowel cancer risk, such as Familial Adenomatous Polyposis (FAP) or Lynch syndrome, you may require screening colonoscopies. Speak to your GP for individual advice and referral to a specialist and Family Cancer Clinic.
| Who will perform the colonoscopy?
Once you’ve been referred by your GP for a colonoscopy, find out who will be performing the procedure. Make sure your colonoscopy will be done by an experienced colonoscopist who is interested in constant improvement in the quality of colonoscopy that he or she provides. Below is a list of questions to ask your colonoscopist to help ensure a high-quality colonoscopy.
How many colonoscopies (%) have you performed in which one or more cancerous polyps (adenomas) were detected?
This percentage is referred to as a Colonoscopist’s Adenoma Detection Rate (ADR) and is considered the measurement that best reflects how carefully colonoscopy is performed.
How many colonoscopies (%) have you performed in which the colonoscope reached the very beginning of the colon (called the 'caecum')?
This percentage is referred to as a Colonoscopist’s caecal intubation rate and is considered an important indicator of colonoscopy quality.
Will my colonoscopy report include photographs of my caecum?
This will illustrate if the full extent of the bowel was examined.
Do you use split-dosing of bowel preparations?
Effective bowel preparation requires that at least half the preparation is ingested on the day of colonoscopy.
Will my colonoscopy report include details about the quality of my bowel preparation?
To ensure effective examination of the bowel it must be prepared according to the instructions accompanying the bowel preparation, otherwise polyps and cancers can be missed, and the colonoscopy may need to be repeated.
Will my colonoscopy report include the colonoscopy withdrawal time?
Longer colonoscopy withdrawal times have been shown to improve polyp detection rates, whereas rapid withdrawal of the colonoscopy may miss polyps and reduce the effectiveness of bowel cancer prevention.

What you can expect from your colonoscopist:
- they are well trained in the procedure and meets agreed standards for competence
- there will be skilful and thorough examination of all parts of the large bowel
- risk factors (e.g. anticoagulant therapy, presence of severe co-morbidities) will be identified well before colonoscopy and action taken to minimise risk
- you will be given a clear explanation of what is involved in the procedure and have an opportunity to ask for more information and that this information will be provided before starting your bowel preparation
- you will be given clear information about the details of the bowel preparation, including the importance of maintaining hydration
- the type of bowel preparation selected for you was based on your personal risk factors (e.g. age, renal impairment) and your personal preference
- the procedure will be performed safely and with minimal discomfort
- verbal and written information about the results of the procedure are given to you
- verbal and written instructions about what to do if problems occur after discharge are provided
- information about follow-up review is given
| How is a colonoscopy performed?
A colonoscopy is conducted in a dedicated, private area with the necessary equipment needed and your vital signs are monitored throughout the procedure by the colonoscopist and medical staff.
You will be lying on your left side on an examination table as you receive sedation intravenously, which will most likely be the last thing you remember about the experience.
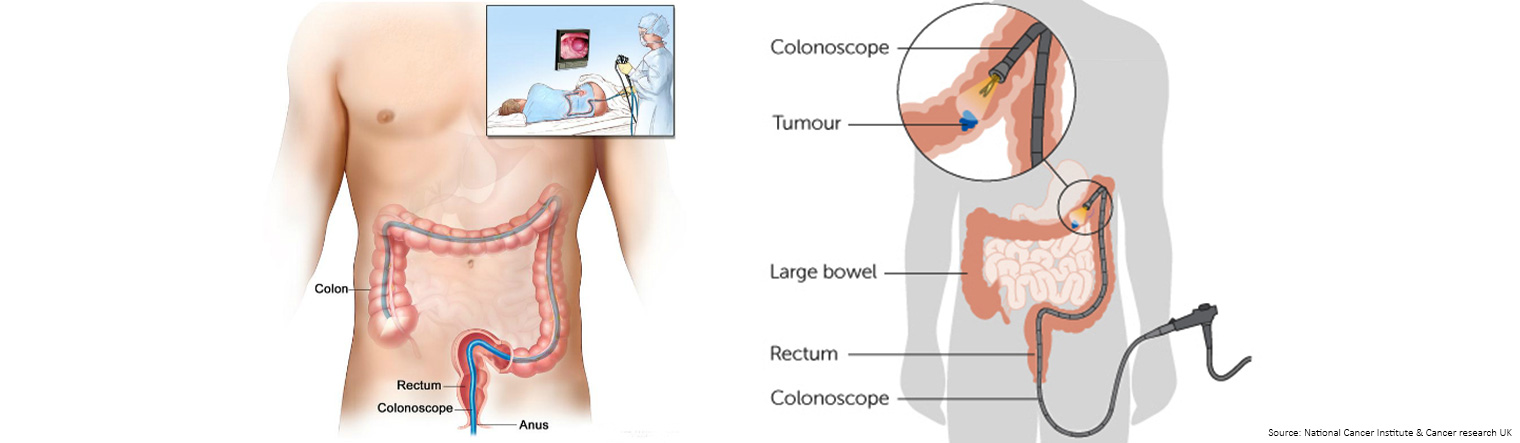
During the procedure, the colonoscopist will insert a tool called a colonoscope into the anus and through the bowel until it reaches the cecum, the area where the small and large intestines meet.
A colonoscope is a long, thin, flexible instrument, connected to a camera with a light source and video display monitor.
The optics of the colonoscope transmit a video image from inside the bowel to a computer screen, and the design of the colonoscope allows for instruments to pass through the channel of the scope to sample or remove tissue, without the need for surgery.
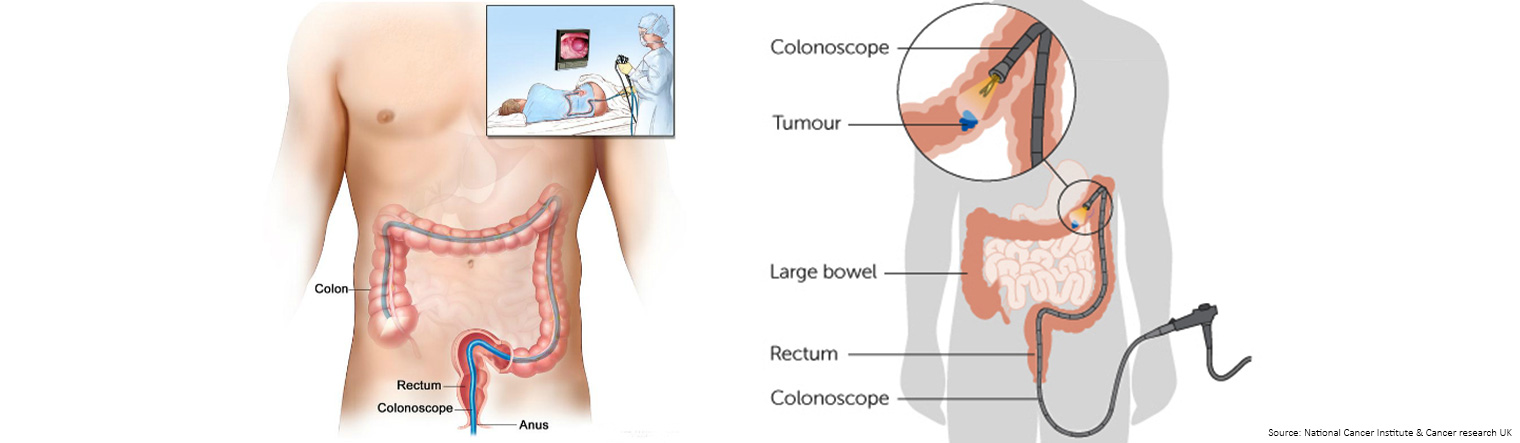
The colonoscope is used to cleanse the surface lining with water, inflate and remove air from the large intestine for an optimal view of the bowel, inspect the bowel lining for abnormalities, take photographs and tissue samples and remove polyps. The procedure to remove polyps is called a polypectomy.
The colonoscopist carefully checks for abnormalities while slowly removing the scope.
If any polyps are found during the procedure, they can usually be removed during the procedure using specialised tools that run inside the colonoscope.
If a polyp or tumour is too big to be safely removed through the colonoscope, the colonoscopist will take a sample of the tissue and send it for testing to determine the nature of the lesion.
If other abnormalities are found in the bowel, or the colonoscopy is being done to determine the cause of symptoms, biopsies will be performed.
Your colonoscopist will discuss the biopsy results with you once a report has been received from the pathologist, which is usually within a week.
At that meeting, it is important to find out the number, size, and pathology of any polyps detected and when you should schedule your next colonoscopy.
| How long does a colonoscopy take?
Colonoscopies usually take place at the hospital’s outpatient department or in a same day procedure centre.
Arrival 30 minutes prior to the procedure allows you to change clothes and get admitted to the pre-procedure room.
The examination generally takes less than half an hour, but the sedative can stay in the blood for up to 24 hours.
Following the procedure you will remain in the recovery area for approximately two hours until the effect of the sedation wears off.
Your vital signs must be acceptable before you will be discharged, but you can return home the same day.
Because of the sedation, you should arrange for someone to collect you and take you home.
The colonoscopist will provide you with a copy of the procedure report, complete with pictures, and tell you if anything was found.
In addition, a letter with the results of any biopsies and the interval for the next colonoscopy will be sent to your mailing address, so it is important that you have provided the most recent information.
If something of concern is discovered, a follow-up plan will be discussed with you.

| Are there any risks related to colonoscopy?
As with any invasive healthcare procedure or examination, there are risks associated with colonoscopy and with preparation for the procedure.
The most common adverse effects associated with colonoscopy include:
- bloating
- nausea
- abdominal pain
- vomiting
Potential risks of colonoscopy can include:
- bleeding
- infection
- intestinal perforation (poking a hole in the bowel)
- not detecting polyps or cancer
- adverse reactions associated with the bowel preparation or sedation
Tips to reduce risks related to colonoscopy and bowel preparation:
- thoroughly discuss and review the condition of your health and any medication (prescription and over-the-counter) that you are taking with your colonoscopist
- ensure the colonoscopist that performs the procedure is an experienced gastroenterologist or surgeon
- follow the bowel preparation directions so that you arrive at the procedure with a clean bowel
| Does a colonoscopy hurt?
Most patients choose to be sedated during a colonoscopy, and wake up in the recovery room with little memory of the procedure.
Because the bowel does not feel pinching or burning sensations, no pain is experienced if the colonoscopist removes polyps or tissue during the procedure.
The colonoscopist will inflate the bowel with air using the colonoscope, in order to get a better view because the bowel is collapsed into a series of folds.
The air can cause a person to feel bloated during or following the procedure, but it will pass naturally.
Your colonoscopist will provide you with a list of written discharge instructions including what symptoms may be normal after colonoscopy and what symptoms should prompt you to call them or seek urgent medical attention.
If you experience severe abdominal pain, excessive rectal bleeding, fever, or anything unanticipated following the procedure, contact your colonoscopist as soon as possible.
| How long does it take to recover from a colonoscopy?
The combination of the bowel preparation process and sedation leaves many patients feeling groggy and weak following the procedure.
As a result, someone must accompany you from the recovery area and take you home following the procedure.
Because you’ve been sedated, you will not be allowed to drive until the next day.
Discharge instructions will be provided by the personnel in the recovery room. They will give you an idea of what to expect over the course of the next day, including restrictions on any medications or activities.
Minor symptoms such as gas or bloating should disappear within 24 hours; however, if you experience pain, bloating, or excessive rectal bleeding following the procedure contact your colonoscopist as soon as possible.
| What is normal and what isn’t following a colonoscopy?
Bowel preparation and colonoscopy can take a temporary toll on the body, so feeling tired following the experience is to be expected.
In addition, it is not uncommon to experience some slight discomfort related to bloating and gas due to air that may still be trapped in the bowel, following the procedure.
Furthermore, if any polyps were removed from the bowel lining, a small ulcer or sore remains at the removal site, which can be prone to bleeding, either immediately or within two weeks.
Before leaving the recovery area, you will also be given phone numbers you can call if any symptoms develop or you have concerns. You will also be provided with a detailed list of discharge instructions which include symptoms you may experience.
However, it’s easier to deal with a problem in its earliest stages, rather than waiting until it gets worse, so speak with your colonoscopist before your discharge about any concerns or symptoms you may have.
Contact your colonoscopist immediately if you experience any of the symptoms listed on your post-colonoscopy discharge sheet, which may include but are not limited to:
- chills or fever
- rectal bleeding (more than a tablespoon)
- swelling or redness at your sedation intravenous (IV) site
- severe abdominal pain or bloating
- persistent nausea or vomiting
- extreme thirst
- dizziness
- headaches
| How long after a colonoscopy do I have to wait before eating and drinking?
Rest and relaxation are generally encouraged for the remainder of the day following your colonoscopy, as are lots of fluids to replace those your body lost during the bowel preparation process.
It is important to rehydrate following bowel preparation and colonoscopy, so you may be asked to avoid drinking alcohol for a few days following the procedure.
In addition, your digestive system may be sensitive following the bowel preparation process. Be gentle when eating your first meal following your colonoscopy and make sure it is something that is easily digestible. Begin slowly, to build up your tolerance.
If your appetite does not return, contact your colonoscopist.
| How long should I wait before resuming my medications after a colonoscopy?
Your colonoscopist may make special recommendations about your use of medications, including over-the-counter medications, herbs, or supplements to minimise the risk of bleeding if you had polyps removed during your colonoscopy.
| How long do I have to wait before I find out my colonoscopy results?
Be sure you, or the person driving you home, get a chance to review the results of the colonoscopy with your colonoscopist before you leave the endoscopy area.
Knowing whether you have something to be concerned about or you’re just expecting a letter to tell you to come back in five years will be reassuring.
Your colonoscopist will be able to reassure or advise you whether there was something serious or concerning detected, immediately after the procedure, even without the results of biopsies.
The majority of individuals undergoing colonoscopy get reassuring news that the procedure was normal or that nothing life threatening was found.
Routine processing of results usually takes less than one week, but if your colonoscopist is concerned about something that was found, the biopsy sample can be rushed through the lab for quicker results.
| My Colonoscopy Experience
If you are aged 18-and-over and have had a colonoscopy, we invite you to provide feedback about your experience.
My Colonoscopy Experience is a user-friendly and easy to understand questionnaire that can be completed anonymously in around 10 minutes.
Developed by Bowel Cancer Australia and powered by Healthie™, the questions ask about your colonoscopy referral, pre-admission, care and treatment, interaction with staff, discharge from care and any post-procedure issues.
Every person’s feedback about their colonoscopy experience is unique and valuable.
Your experience with the health system is an important and meaningful measure of quality of care that can be used for performance monitoring purposes and to drive quality improvement.
Measuring patient colonoscopy experience in Australia is long overdue.
Help us ensure the patient voice is heard, so that future colonoscopy care reflects what patients want and need.
Together, we can make real change happen!
Please click on the image below to share your anonymous feedback or contact Bowel Cancer Australia on 1800 555 494 for more information.