Dedicated to leading edge bowel cancer discoveries
Researching a cure for Australia's second deadliest cancer is to receive a major boost with $10.4 million to establish a professorial chair of bowel cancer research at the University of Sydney.
The majority of funding comes from national charity Bowel Cancer Australia, which has committed $6.4 million to establish the position and will be supported by additional funds of $4 million available to the University to advance research into bowel cancer.
Bowel Cancer Australia chairman Craig Jackson said that the establishment of the chair at the University of Sydney was the culmination of many years of effort by the Bowel Cancer Australia Board.
An endowed professorial chair is recognised as a University's finest scholar in their field of expertise. They provide a research focal point in the country they are located, helping to attract and retain the brightest researchers and spur colleagues to their finest efforts - benefiting the entire Australian community.
To underscore the significance of this research investment, expenditure by the National Health & Medical Research Council (NHMRC) on bowel cancer was $12.3 million in 2017.
Bowel Cancer Australia chief executive Mr Julien Wiggins said the size of the funding commitment will enable the chair and ancillary support to continue in perpetuity.
"Our funding will expand Australia's research capacity and we anticipate the Chair will be a game changer for bowel cancer research in this country," he added.
Bowel cancer is the second deadliest cancer in Australia, claiming more than 5,000 lives each year.
"Changing that will require significant, long-term funding for dedicated bowel cancer research and that's what we've provided."
"While screening can help with early detection, it won't eliminate bowel cancer. Research is the only way to discover a cure," said Mr Wiggins.
The Lawrence Penn Chair of Bowel Cancer Research is named after one of Australia's oldest bowel cancer survivors and is based at the University of Sydney's Northern Clinical School Campus.
"We are extraordinarily grateful to Bowel Cancer Australia for their support," said the Dean of Sydney Medical School, Professor Arthur Conigrave.
"In times when national research funding is increasingly difficult to secure, we rely more than ever on funds from community groups and individuals to undertake the research which is essential if we are to better prevent and treat bowel cancer.
"The University of Sydney has many world-class cancer researchers and clinicians. This philanthropic support for bowel cancer means we can build on our existing programs and make a greater contribution to improving cancer outcomes," said Professor Conigrave.
Bowel Cancer Australia relies solely on the generosity of community and corporate supporters as it receives no government funding.
Please support Bowel Cancer Australia's ongoing research efforts to help save lives and to improve the health and wellbeing of people living with bowel cancer.
To make a donation please call 1800 555 494 or click here.
The majority of funding comes from national charity Bowel Cancer Australia, which has committed $6.4 million to establish the position and will be supported by additional funds of $4 million available to the University to advance research into bowel cancer.
Bowel Cancer Australia chairman Craig Jackson said that the establishment of the chair at the University of Sydney was the culmination of many years of effort by the Bowel Cancer Australia Board.
An endowed professorial chair is recognised as a University's finest scholar in their field of expertise. They provide a research focal point in the country they are located, helping to attract and retain the brightest researchers and spur colleagues to their finest efforts - benefiting the entire Australian community.
To underscore the significance of this research investment, expenditure by the National Health & Medical Research Council (NHMRC) on bowel cancer was $12.3 million in 2017.
Bowel Cancer Australia chief executive Mr Julien Wiggins said the size of the funding commitment will enable the chair and ancillary support to continue in perpetuity.
"Our funding will expand Australia's research capacity and we anticipate the Chair will be a game changer for bowel cancer research in this country," he added.
Bowel cancer is the second deadliest cancer in Australia, claiming more than 5,000 lives each year.
"Changing that will require significant, long-term funding for dedicated bowel cancer research and that's what we've provided."
"While screening can help with early detection, it won't eliminate bowel cancer. Research is the only way to discover a cure," said Mr Wiggins.
The Lawrence Penn Chair of Bowel Cancer Research is named after one of Australia's oldest bowel cancer survivors and is based at the University of Sydney's Northern Clinical School Campus.
"We are extraordinarily grateful to Bowel Cancer Australia for their support," said the Dean of Sydney Medical School, Professor Arthur Conigrave.
"In times when national research funding is increasingly difficult to secure, we rely more than ever on funds from community groups and individuals to undertake the research which is essential if we are to better prevent and treat bowel cancer.
"The University of Sydney has many world-class cancer researchers and clinicians. This philanthropic support for bowel cancer means we can build on our existing programs and make a greater contribution to improving cancer outcomes," said Professor Conigrave.
Bowel Cancer Australia relies solely on the generosity of community and corporate supporters as it receives no government funding.
Please support Bowel Cancer Australia's ongoing research efforts to help save lives and to improve the health and wellbeing of people living with bowel cancer.
To make a donation please call 1800 555 494 or click here.
| Professor Mark Molloy PhD
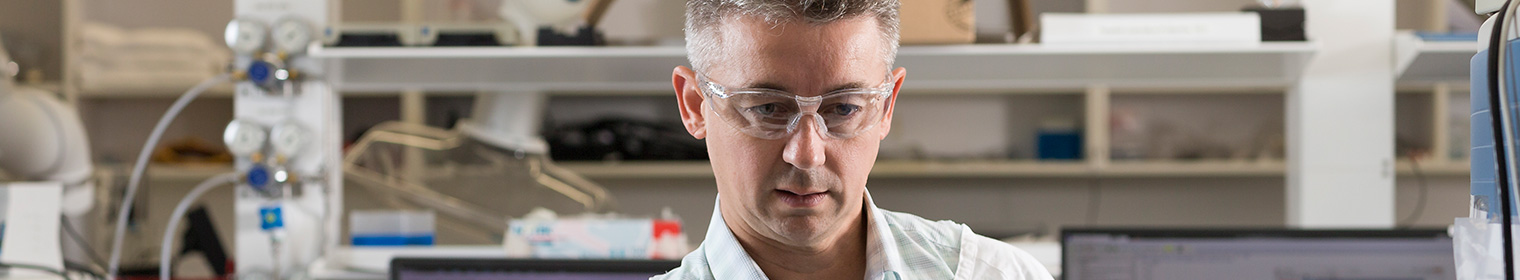
Professor Mark Molloy PhD is the inaugural Lawrence Penn Chair of Bowel Cancer Research, located at the Kolling Institute, on the Royal North Shore Hospital Campus.
Professor Molloy is the leader researcher of The Bowel Cancer and Biomarker Research Group which focuses on translational cancer research working at the interface of science and clinical research. The Group apply scientific expertise to questions of clinical relevance that will improve the care of bowel cancer patients.
Professor Molloy is a biochemist and has developed his expertise in the science of 'proteomics'. He is internationally recognised as an expert in the application of mass spectrometry in biomedical research. Professor Molloy’s focus areas are in translational cancer research, biomarker studies and cell signalling.
A major theme of Professor Molloy’s research has been to use mass spectrometry to conduct quantitative proteomic analyses of biospecimens. He has used this approach for the molecular characterisation of colon, thyroid and pancreatic cancers, melanomas and some lung cancers. The data has been used to identify prognostic and predictive protein biomarkers.
More recently, Professor Molloy has opened a new research direction to use mass spectrometry for pharmacokinetic monitoring of cancer drug levels in patients and to explore analysis from dried blood spots. Many of these collaborations have been with clinicians. This new role will enable him to expand these interactions and focus a major effort towards molecular analysis of bowel cancer.
Professor Molloy completed his PhD in proteomic sciences at Macquarie University in 2000 under the supervision of Keith Williams, co-inventor of the term "proteomics" before conducting post-doctoral research at the University of Michigan Medical School in Ann Arbor, USA. He then worked in the US at Pfizer Inc for four years applying biomarker research to support new drug development.
Professor Molloy returned to Australia to take up a National Health and Medical Research Council career development award fellowship on colorectal cancer biomarker proteins in collaboration with Professor Stephen Clarke, before becoming Director of APAF.
Professor Molloy’s leadership and international standing in the application of proteomics is evidenced by outstanding grant success (career total $42.9M), publications (>150), Scopus citations (>4900) and HDR student completions (14). He is a Chief Investigator of the Sydney Vital Translational Cancer Research Centre.
The commencement of Professor Molloy as the Lawrence Penn Chair of Bowel Cancer Research is the culmination of many years of hard work by all concerned and marks the beginning of many more years of valuable, translatable research.
The establishment of the Chair at the University of Sydney provides a unique opportunity to build a research team committed to beating bowel cancer, a disease which is projected to claim the lives of 33,964 Australians in the next seven years.
| Proteomoics
Professor Molloy will be applying molecular technologies to discover what causes a polyp to become cancerous and what drives the spread of disease.
Molecular technologies include genomics (the study of all the genes), proteomics (the study of all the proteins), and metabolomics (the study of all the metabolites).
To understand the biology underlying cancer, scientists have traditionally studied cancer genes – the genome. That analysis has shown that bowel cancers are not uniform and can be subdivided into at least four types, based on molecular features they possess.
However, a blind spot in research has been the study of all the proteins – the proteome – which is the molecular machinery of the cell.
Cancer proteomics is an important new frontier in cancer research. It uses mass spectrometry, a powerful analytical technique for identifying proteins and measuring the quantity of each type of protein that is present.
"We need to look at the things that the genes are producing, and that's what proteomics is about," explained Professor Molloy.
"By studying how protein structure and function change when diseases such as cancer are present, we are hoping to identify which specific proteins play a role in bowel cancer," Professor Molloy added.
Knowing which proteins are present in bowel cancer is essential for developing new cancer treatments and for using existing treatments as efficiently as possible because most of the drugs used to treat diseases such as cancer interact with proteins.

| Mass spectrometry
Professor Molloy’s focus is on molecular analysis, which can improve understanding of tumour biology and help clinicians make decisions about treatment. It is an area of research that could have a profound impact on the care of bowel cancer patients.
“There is no doubt that technology is driving a big revolution in clinical care,” Professor Molloy said.
One example of this technological transformation is the use of mass spectrometers – sophisticated weighing devices that allow researchers to determine the molecular make-up of various substances.
With two new mass spectrometers installed at the Kolling Institute, Professor Molloy and his team will analyse the molecular features of proteins and metabolites in individual tumours, to tailor treatment pathways according to the needs of each patient.
"When combined with genomic analysis, this gives us a more complete molecular picture of bowel cancer, which is essential to better understand prevention and treatment strategies," Professor Molloy said.
Mass spectrometers could also be used to monitor medication levels in a patient’s system, allowing clinicians to deliver a dose precisely calibrated to suit the individual.
Mass spectrometers could also be used to monitor medication levels in a patient’s system, allowing clinicians to deliver a dose precisely calibrated to suit the individual.
“Currently those decisions are based on BMI [body mass index],” said Professor Molloy.
“But people metabolise these drugs differently based on genetics … By applying molecular analysis techniques to blood samples, the oncologist could potentially adjust the medication levels up or down in a more precise and personalised way.”
The goal is to find ways of integrating molecular analysis into everyday patient care. Professor Molloy envisages that within the next five years clinical teams working with bowel cancer patients could include a molecular scientist.
The goal is to find ways of integrating molecular analysis into everyday patient care. Professor Molloy envisages that within the next five years clinical teams working with bowel cancer patients could include a molecular scientist.
“Today, these multidisciplinary teams discuss imaging, surgery, approaches to chemotherapy and so on,” he said.
“I’d like to see clinicians also asking how molecular analysis could help add to the fuller picture.”

| Lawrence Penn
The Chair of Bowel Cancer at the University of Sydney is named after Mr Lawrence Penn, one of Australia’s oldest bowel cancer survivors. Passionate aviator, former RAAF and Qantas pilot, Lawrence Penn was one of approximately 7,000 Australians diagnosed with bowel cancer in 1985.
At the time, the five-year relative survival rate was just 47 percent and life expectancy for newly diagnosed bowel cancer patients with advanced disease was just five months. With improvements in early detection, advances in surgery and effective adjuvant chemotherapy to prevent cancer recurrence, an increasing number of advanced bowel cancer survivors are living longer.
Unfortunately, while mortality rates are remaining stable, and in some age-groups declining, incidence is forecast to rise to 20,000 new cases per year by 2020. For those who detect the disease early like Mr Penn, 90 percent of bowel cancer cases can be successfully treated.
“I feel very honoured to think my name is going to be associated with such important research,” Mr Penn said.
Because of his family’s experience with bowel cancer, Lawrence Penn’s son Richard and wife Heather, became active supporters of Bowel Cancer Australia’s work.
Mr Richard Penn, Chairman of the Penn Foundation, was invited by the Board to become Patron of Bowel Cancer Australia in 2006. One year later, The Penn Foundation helped launch a fundraising appeal to establish Australia’s first Chair of Bowel Cancer Research, with a $1million funding commitment.
“My main motivation for getting this chair was so as many people as possible can have more time with their loved ones,” Richard said.
| Sustainable funding to expand Australia's bowel cancer research capacity
Bowel cancer is Australia's second deadliest cancer and has the second highest disease burden of any cancer in Australia.
Burden of disease measures the impact of living with illness and injury or dying prematurely.
However, bowel cancer received around 55 percent less research funding from the National Health and Medical Research Council (NHMRC) compared to breast cancer (2021: $8.6 million v $19.1 million); and receives no government funding to support dedicated Bowel Care Nurse Specialists, compared to $120 million for 98 Breast Care Nurse Specialists; $33 million for 62 Prostate Cancer Nurse Specialists, and $6.9 million for 5 Lung Cancer Nurse Specialists.
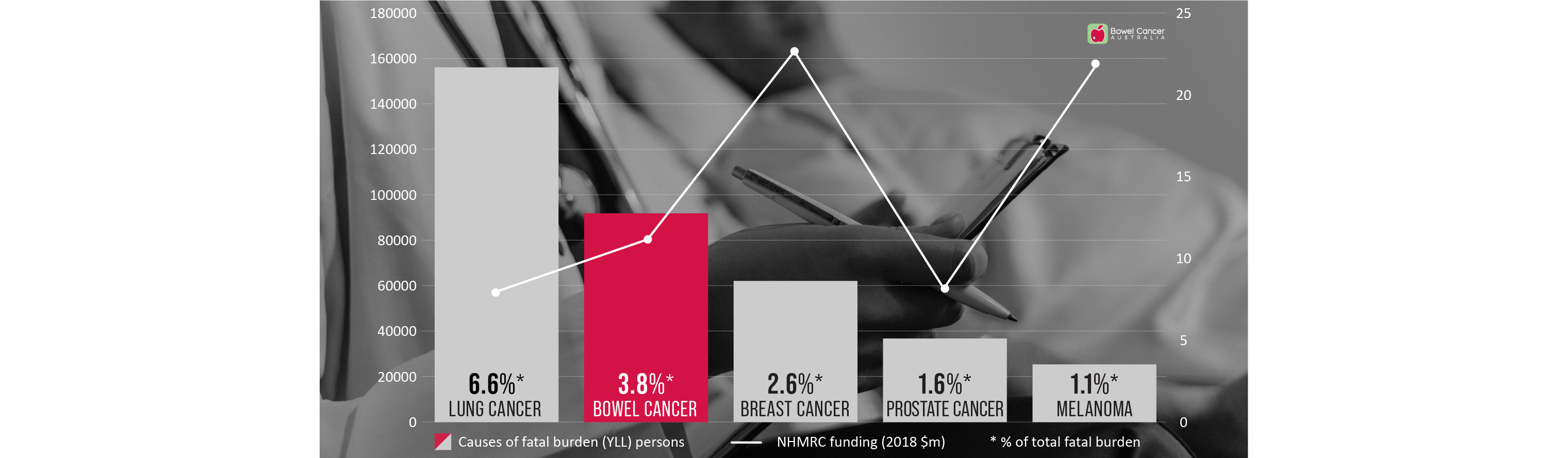
Burden of disease measures the impact of living with illness and injury or dying prematurely.
However, bowel cancer received around 55 percent less research funding from the National Health and Medical Research Council (NHMRC) compared to breast cancer (2021: $8.6 million v $19.1 million); and receives no government funding to support dedicated Bowel Care Nurse Specialists, compared to $120 million for 98 Breast Care Nurse Specialists; $33 million for 62 Prostate Cancer Nurse Specialists, and $6.9 million for 5 Lung Cancer Nurse Specialists.
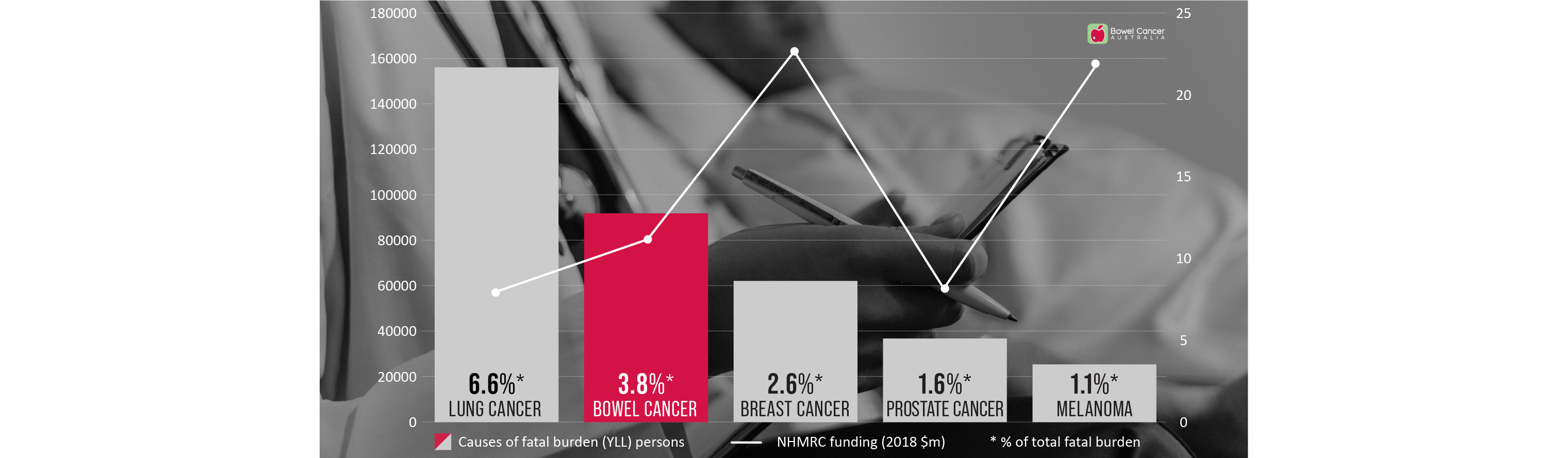
To help address this research funding inequity, Bowel Cancer Australia established the Bowel Cancer Research Foundation Australia.
An objective of the Foundation is to support and sustainably fund research into the causes, prevention and treatment of bowel cancer to benefit us all in the future. While Bowel Cancer Australia is here today supporting, informing and caring for people affected by the disease.
Through the Foundation, Bowel Cancer Australia has made a significant investment in the Lawrence Penn Chair of Bowel Cancer Research, dedicated to leading edge bowel cancer discoveries that aim to have an everlasting impact on Australia's health future.
The establishment of the Lawrence Penn Chair, in collaboration with the University of Sydney and the Kolling Institute, strengthens our collective pursuit of a bowel cancer cure.
Other major bowel cancer projects funded to date, include the ASCOLT Clinical Trial; ICHOM Colorectal Cancer Standard Set; patient-reported experiences (My Colonoscopy Experience), community awareness and understanding; patient and metastatic patient lived-experiences; and demographic research.
To date, Bowel Cancer Australia, collaboratively with funding partners, has funded over $12.5 million in bowel cancer research projects.
You can make a lasting contribution to bowel cancer research through a donation or a bequest (a gift made in your Will) to Bowel Cancer Australia or by calling us on 1800 727 336.

Through the Foundation, Bowel Cancer Australia has made a significant investment in the Lawrence Penn Chair of Bowel Cancer Research, dedicated to leading edge bowel cancer discoveries that aim to have an everlasting impact on Australia's health future.
The establishment of the Lawrence Penn Chair, in collaboration with the University of Sydney and the Kolling Institute, strengthens our collective pursuit of a bowel cancer cure.
Other major bowel cancer projects funded to date, include the ASCOLT Clinical Trial; ICHOM Colorectal Cancer Standard Set; patient-reported experiences (My Colonoscopy Experience), community awareness and understanding; patient and metastatic patient lived-experiences; and demographic research.
To date, Bowel Cancer Australia, collaboratively with funding partners, has funded over $12.5 million in bowel cancer research projects.
You can make a lasting contribution to bowel cancer research through a donation or a bequest (a gift made in your Will) to Bowel Cancer Australia or by calling us on 1800 727 336.

| Researching improved follow-up colonoscopy surveillance timings
Profiling of 60 bowel adenoma polyps will be used to better define optimal colonoscopic surveillance intervals, thanks to a new research grant to the Lawrence Penn Chair of Bowel Cancer Research from the Medical Research Future Fund (Sydney Health Partners).
Professor Mark Molloy, and his collaborators including Professor Alexander Engel from Royal North Shore Hospital will use molecular analysis of bowel polyps to investigate disease risk, seeking to find a signature of transformation risk which could potentially be used to optimise colonoscopy surveillance intervals.
"The research grant provided by the Medical Research Future Fund is exciting as it allows us to trial a pathway for molecular testing of bowel polyps and see if this information can tell us more about a given patient's bowel cancer risk,” said Professor Mark Molloy.
“It may offer an opportunity for more personalised prognosis as we will consider genetic, proteomic and microbiome features of these precancerous growths, which are not currently part of routine pathology testing," he added.
Researchers will use the local health district colonoscopy screening clinic to collect and analyse up to 60 polyps of varying risk levels.
"We will also explore if this molecular information may be useful for guiding follow-up colonoscopy surveillance timing as this would help improve scheduling and costs," Professor Molloy said.

| Researching why some early stage bowel tumours metastasise to lymph nodes
Funding from the Colorectal Surgical Society ANZ Foundation will support new research to improve our understanding of why some early stage bowel tumours metastasise to lymph nodes.
“This is important because patients with lymph node disease have worse prognosis and face more intense treatment than patients whose cancer remains within the bowel wall,” said Lawrence Penn Chair of Bowel Cancer Research Professor Mark Molloy.
The $60,000 research grant awarded to the Chair will enable molecular analysis to refine risk of dissemination in early stage tumours and transformation potential of some bowel polyps.
“Patients with Stage I bowel cancer have a greater than 98% 5-year rate of survival which falls to around 70% when the tumour has metastasized to lymph nodes,” Professor Molloy said.
“We need to better understand this process to develop medical interventions and stop the tumour disseminating elsewhere," he added.
The project will generate preliminary data using genomic sequencing of early stage tumours and malignant bowel polyps. Professor Molloy and his team aim to link these mutations with those early tumours which spread to lymph nodes, providing a biomarker of risk which may inform surgical pathways.

| Dr Mudy De Silva awarded the Penelope Morris Foundation Scholarship
Dr Mudy De Silva is a Medical Oncologist with a special interest in clinical trials and translational research in gastrointestinal cancers.
While doing clinical training Medical Oncology at Royal North Shore Hospital in Sydney, he developed a strong interest in bowel cancer.
“What I find interesting and challenging about bowel cancer research is the complex interplay of tumour, genes, gut microbiome, and the immune system,” said Mudy.
Mudy is also curious as to why immunotherapies, which have led to landmark survival rates in several other cancers, do not appear to be effective for most patients with bowel cancer.
“Furthermore, there is an alarming trend indicating young onset bowel cancers are on the rise,” said Mudy.
“Personally, I have come across many younger patients with bowel cancer at various stages, including two young women who were diagnosed with metastatic disease during pregnancy.”
“These latter cases have impressed upon me the need to understand more about the biology, behaviour, and management of bowel malignancies.”
As the recipient of the highly coveted Penelope Morris Foundation PhD scholarship offered through The University of Sydney, Mudy will be able to focus his studies on the molecular analysis of young onset bowel cancer under the supervision of Lawrence Penn Chair Professor Mark Molloy and eminent medical oncologist, Professor Stephen Clarke.
“It is an absolute pleasure to be involved with translation research in bowel cancer, and I am deeply grateful to Professor Mark Molloy as well as the Penelope Morris Foundation for facilitating this work,” Mudy said.
“I sincerely hope to bring discoveries from our lab to the clinic and translating them into clinically meaningful benefits for patients.”
“Despite significant improvements over the past 4 to 5 decades, the 5-year overall survival of patients with metastatic disease remains poor at around 15%.”
“Furthermore, data from registries of real-world patients suggest there has been no improvement in overall survival for patients with metastatic disease since 2008.”
“At present, we give empirical therapies to patients with bowel cancer based on just a few biomarkers, highlighting the significant need for discovery of novel biomarkers and therapeutic strategies through translational research,” said Mudy.
“We now have a better understanding that the clinical activity of many cancer therapies can be attributed to the re-establishment of immune surveillance within the tumour microenvironment through a specific type of immunogenic cell death (ICD).”
“ICD is unique to other forms of regulated cell death and necrosis in that it produces a robust anti-tumour adaptive immune response, which can be lasting.”
“There are several hallmarks of ICD, and I am keen to explore whether these are detectable with currently available technologies, and whether they have prognostic or predictive value as biomarkers.”
Mudy will also be exploring which treatment strategies optimise immunogenic cell death, in order to better understand how cancers develop resistance to it.

| Dr Zoe Welham awarded The Penn Foundation Scholarship
Zoe developed an interest in bowel cancer while she was working on a complex scientific research project in graduate school.
“The goal was to look at bowel cancer in a holistic way by taking information from genes, microbes and epigenetic data,” Zoe said.
As a PhD recipient of The Penn Foundation Scholarship at The University of Sydney, Zoe will now be able to build on that analysis under the supervision of the Lawrence Penn Chair of Bowel Cancer Research, Professor Mark Molloy.
Zoe will compare the microbiomes of polyps at different risk levels for developing bowel cancer, to better understand how the gut microbiome influences the growth of bowel polyps.
She will also investigate the metabolites these microbes produce (such as butyrate, which is thought to be an important energy source for colon epithelia), to see how they correlate with polyp risk.
She will then study ways to integrate this data with other molecular features and with the patient’s medical history.
Through her research, Zoe aims to provide valuable new knowledge regarding the biological rules that govern bowel polyp growth – something which is still not fully understood.
“The gut microbiome is interesting because of how it appears to play a role in a wide range of health issues, from food metabolism, to interacting with our immune system, and even influencing neurological traits,” said Zoe.
“Humans enjoy a symbiotic relationship with our bugs."
“We provide food and they help with food digestion and provide molecules that influence many of our body processes."
“I also find it interesting that, unlike our genes, we can control what bugs make up our microbiomes to some an extent – simply by changing our diets."
“For example, research suggests that people with high meat intake have different ratios of gut bacteria to people who eat less meat."
“This is interesting, given excess red meat consumption is a risk factor for bowel cancer.”
Zoe hopes her work will ultimately lead to a reduction in bowel cancer.
Benita is a junior post-doctoral fellow and Immunologist who is helping identify new ways to regulate polyp development through microscopy assays that phenotype the different immune cells in polyps and surrounding mucosa.
| Dr Pascal Steffen awarded Early Career Fellowship
A new grant secured by the Lawrence Penn Chair of Bowel Cancer Research laboratory from the Cancer Institute NSW will enable further investigation into the prognostic contribution of immune cell infiltration in rectal cancer.
The $600,000 grant will provide a three-year fellowship salary for Dr Pascal Steffen and help to cover some research costs for him to apply proteomic techniques to investigate the role of immune cells in rectal cancer.
Approximately 5,000 Australian men and women are diagnosed with rectal cancer each year. The aim of Dr Steffen’s CINSW fellowship is to understand the involvement of immune cell infiltration in rectal cancer, how this impacts tumour biology and how it affects patient outcomes.
To conduct the study over the next three years, Dr Steffen will apply his knowledge of protein mass spectrometry with access to the large archival rectal cancer tissue database at Royal North Shore Hospital. He will map the proteome (proteins found in the cancer) of these rectal cancers to understand their biology and how this links to patient prognosis, and work to resolve the complex immune cell architecture of these cancers by using a new technique of imaging mass cytometry.
The outcome of this research will lead to new prognostic biomarker panels, provide a better understanding of immune cells in rectal cancers and pave the way for new treatments.
“I am very excited to receive the CINSW fellowship as it will allow me to apply my expertise in proteomics to the cause of advancing the understanding of the role of immune cells in rectal cancer and furthering the research of new ways to combat this disease. This fellowship will also grant me the opportunity to broaden my knowledge especially in the field of immunology and imaging techniques,” said Dr Steffen.
Dr Pascal Steffen will conduct his fellowship in the Bowel Cancer and Biomarker Laboratory at The Kolling Institute, Royal North Shore Hospital in Sydney under the supervision of Professor Mark Molloy, Lawrence Penn Chair of Bowel Cancer Research, The University of Sydney.
“One of the key objectives for the Chair of Bowel Cancer Research is to increase research capacity and foster researcher development. I am delighted that the CINSW is supporting our vision through the award of this prestigious fellowship to Pascal. His research will reveal important new understandings in rectal cancer which is an essential step towards improving the outcomes for people with this disease,” Professor Molloy said.
Dr Pascal Steffen is a post-doctoral research associate (early career research fellow) and the newest member of the team working with the Lawrence Penn Chair of Bowel Cancer Research, Professor Mark Molloy.
The $600,000 grant will provide a three-year fellowship salary for Dr Pascal Steffen and help to cover some research costs for him to apply proteomic techniques to investigate the role of immune cells in rectal cancer.
Approximately 5,000 Australian men and women are diagnosed with rectal cancer each year. The aim of Dr Steffen’s CINSW fellowship is to understand the involvement of immune cell infiltration in rectal cancer, how this impacts tumour biology and how it affects patient outcomes.
To conduct the study over the next three years, Dr Steffen will apply his knowledge of protein mass spectrometry with access to the large archival rectal cancer tissue database at Royal North Shore Hospital. He will map the proteome (proteins found in the cancer) of these rectal cancers to understand their biology and how this links to patient prognosis, and work to resolve the complex immune cell architecture of these cancers by using a new technique of imaging mass cytometry.
The outcome of this research will lead to new prognostic biomarker panels, provide a better understanding of immune cells in rectal cancers and pave the way for new treatments.
“I am very excited to receive the CINSW fellowship as it will allow me to apply my expertise in proteomics to the cause of advancing the understanding of the role of immune cells in rectal cancer and furthering the research of new ways to combat this disease. This fellowship will also grant me the opportunity to broaden my knowledge especially in the field of immunology and imaging techniques,” said Dr Steffen.
Dr Pascal Steffen will conduct his fellowship in the Bowel Cancer and Biomarker Laboratory at The Kolling Institute, Royal North Shore Hospital in Sydney under the supervision of Professor Mark Molloy, Lawrence Penn Chair of Bowel Cancer Research, The University of Sydney.
“One of the key objectives for the Chair of Bowel Cancer Research is to increase research capacity and foster researcher development. I am delighted that the CINSW is supporting our vision through the award of this prestigious fellowship to Pascal. His research will reveal important new understandings in rectal cancer which is an essential step towards improving the outcomes for people with this disease,” Professor Molloy said.
Dr Pascal Steffen is a post-doctoral research associate (early career research fellow) and the newest member of the team working with the Lawrence Penn Chair of Bowel Cancer Research, Professor Mark Molloy.
| Mass spectrometry core facility opens
Professor Molloy’s focus is on molecular analysis, which can improve understanding of tumour biology and help clinicians make decisions about treatment. It is an area of research that could have a profound impact on the care of bowel cancer patients.
“There is no doubt that technology is driving a big revolution in clinical care,” Professor Molloy said.
One example of this technological transformation is the use of mass spectrometers – sophisticated weighing devices that allow researchers to determine the molecular make-up of various substances.
With two new mass spectrometers installed at the Kolling Institute, Professor Molloy and his team will analyse the molecular features of proteins and metabolites in individual tumours, to tailor treatment pathways according to the needs of each patient.
"When combined with genomic analysis, this gives us a more complete molecular picture of bowel cancer, which is essential to better understand prevention and treatment strategies," Professor Molloy said.
Mass spectrometers could also be used to monitor medication levels in a patient’s body, allowing clinicians to deliver a dose precisely calibrated to suit the individual patient.
The goal is to find ways of integrating molecular analysis into everyday patient care. Professor Molloy envisages that within the next five years clinical teams working with bowel cancer patients could include a molecular scientist.
“Today, these multidisciplinary teams discuss imaging, surgery, approaches to chemotherapy and so on,” he said.
“I’d like to see clinicians also asking how molecular analysis could help add to the fuller picture.”
At the opening of the new facility earlier this month, Professor Molloy explained how the two state-of-the-art mass spectrometry instruments would underpin his research team's effort to map the proteome (the proteins) and metabolome (the metabolites) from specimens provided by bowel cancer patients.
The facility was made possible with a significant financial gift of $500,000 from Bowel Cancer Australia and the Bowel Cancer Research Foundation Australia.
“These new mass spectrometers will have a profound impact on the future of patient treatment and care by allowing researchers to more closely examine bowel polyps, precancerous growths that can grow into cancers, to better understand why they develop in some people,” said Professor Molloy.
Professor Molloy demonstrated how the mass spectrometer can map the proteome using a very small amount of bowel cancer on a pathology slide, revealing the instrument’s incredible capabilities in providing biological information compared to older systems.
“This is viewed as a key aspect of understanding the triggers that allow bowel cancers to grow and metastasize to other body locations,” he added.
Research undertaken by the Lawrence Penn Chair of Bowel Cancer Research is aiming to give new information to clinicians that will better inform them of appropriate treatment pathways based on the molecular information encoded in a patient’s polyp or tumour.
The Lawrence Penn Chair continues to emphasise the importance of research to understand ways we can prevent bowel cancer and to lead the way in providing better treatments for bowel cancer patients.