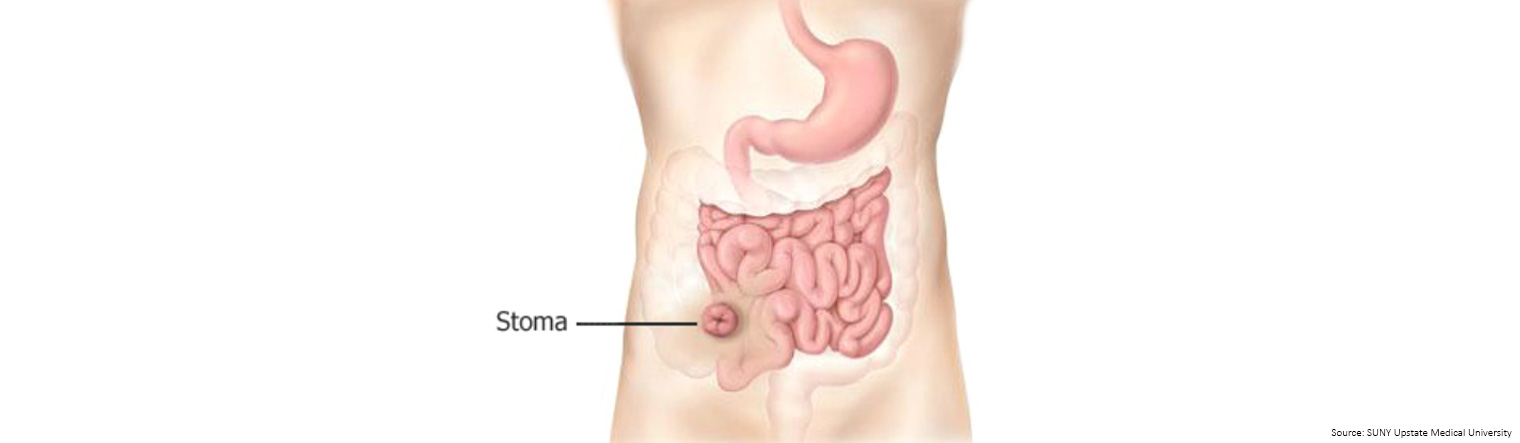
Sometimes, during surgery, it may be necessary for the surgeon to form an artificial opening on the the wall of your abdomen called a 'stoma' to collect waste.
The stoma may be temporary (to allow the bowel time to heal) or permanent.
There are different types of stoma and, if you need one, the type you have depends on the location of your tumour and the type of surgery you need.
The stoma may be temporary (to allow the bowel time to heal) or permanent.
There are different types of stoma and, if you need one, the type you have depends on the location of your tumour and the type of surgery you need.
An 'ileostomy' is a stoma formed by bringing the end or loop of small bowel (the ileum) out on to the surface of your abdomen.
If possible, you may be able to agree on a site for your stoma with your stoma nurse before your operation. This is usually made on the right-hand side of your body, but may in some circumstances be on the left-hand side.
The stoma will be moist and pinkish red in colour and will protrude slightly from your abdomen.
It may be quite swollen to begin with but will reduce in size over time – usually after 6-8 weeks.
Despite being red, there is no sensation in the stoma and it's not painful.
The intestinal waste passes out of the ileostomy and is collected in an external pouching system (generally known as an ileostomy bag).
Ileostomies can be formed during surgery to allow the colon to rest and heal following your surgery. Usually, following a period of 8–10 weeks, the ileostomy is reversed and you go back to using your bowels in the usual way.
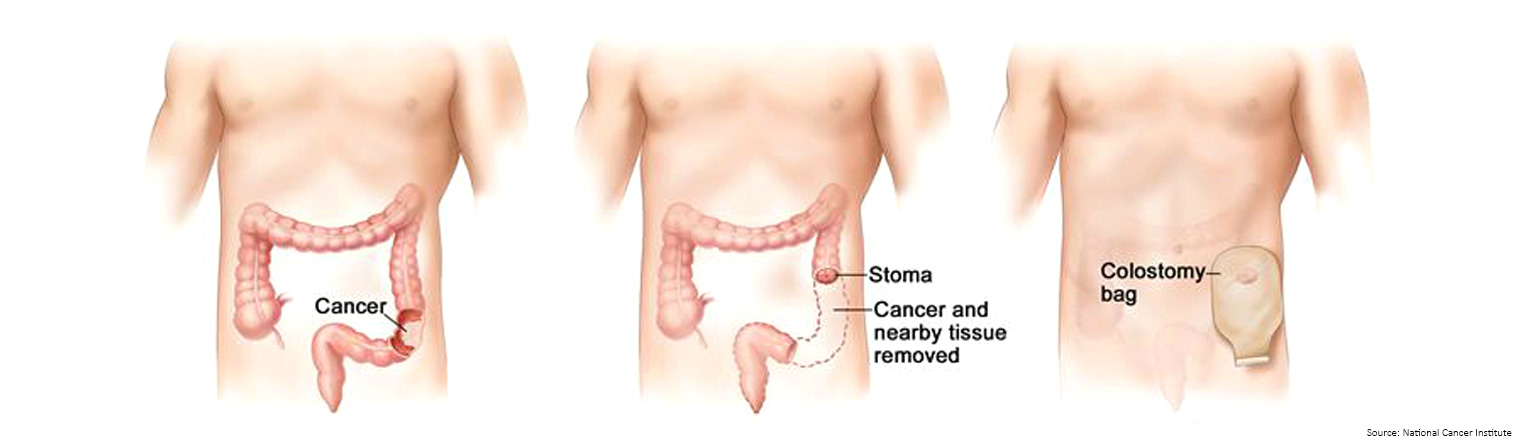
A 'colostomy' is a stoma formed by bringing part of your colon (large bowel) out on to the surface of your abdomen.
If possible, you may be able to agree on a site for your stoma with your stoma nurse before your operation. The opening is usually made on the left-hand side of your body, but may in some circumstances be on the right-hand side.
The stoma will be moist and pinkish red in colour and will protrude slightly from your abdomen.
It may be quite swollen to begin with but will reduce in size over time – usually after 6-8 weeks.
Despite being red, there is no sensation in the stoma and it's not painful.
The intestinal waste, (which is 'formed' having passed through the colon where water is absorbed) passes out of the colostomy and is collected in an external pouching system (generally known as a colostomy bag).
A temporary colostomy can be formed to 're-route' poo away from the section of the colon which has been operated on.
A second operation is later carried out to reverse the stoma and allow the patient to resume normal bowel function.
Permanent colostomies also need to be formed for some patients if the surgeon is unable to join the ends of the bowel that are left or if your anus needs to removed due to the location of the tumour.
Your surgeon will tell you before surgery, during the consent process, if you might need a stoma to be formed.
It's not always possible to know 100 percent either way as the decision is often made during the surgery once the surgeon can see the tumour and what needs to be surgically removed.
You may meet with the stoma nurse before the surgery who is a specialist in caring for patients who require a stoma.
They will discuss with you where the stoma will be on your abdomen and answer any questions or concerns you have.

You will meet with the stoma nurse again after the operation. They understand it can be very daunting at first and that learning to manage your stoma will take time and practice.
No-one expects you to be an expert overnight.
For the first few days, the stoma nurse and the nurses on the ward will help you with your stoma.
As soon as you are well enough, the stoma nurse will show you how to clean your stoma, and how to change the bag.
They will give you hints and tips on how to independently manage your stoma, including how to be thoroughly prepared before you start changing the bag so you know you have everything you need to hand in the bathroom. If appropriate, they may also talk to you about irrigation as a method of managing your stoma (colostomies only) instead of wearing a bag.
They will also talk to you about the different types of appliances (bags) that are available and which one might be best for you.
It might be useful to have a relative or friend with you at this time in case you need help or support when you get home.
Once you are able to manage your stoma independently and the medical team are happy with you, you will be discharged home. Your stoma nurse will ensure you have a plentiful supply of stoma bags to go home with and explain how to order more products as required.
After surgery some people can eat normal foods and have normal output from their stoma. However, some people experience loose bowel motions or constipation (blockage). The low fibre diet is often suggested for people with a stoma who are experiencing difficult bowel motions and for some people temporarily after a stoma reversal. Visit our ostomy low fibre diet webpage for more information and recipes.
Download or order a copy of Bowel Cancer Australia's Ileostomy & Colostomy booklet, which provides essential advice for before and after your operation and has been written to answer some of the questions often asked about having an ileostomy or colostomy.
Stoma Appliance Scheme for ostomates
The Stoma Appliance Scheme supports around 50,000 Australians with a stoma or fistula that facilitates the removal of urine and/or products of the gastrointestinal tract from the body. Find out how to access the scheme, how to select your stoma products and how to order.
Continence Aids Payment Scheme (CAPS)
The Continence Aids Payment Scheme provides a payment to eligible people, to help with some of the costs of buying continence products.
The Continence Aids Payment Scheme provides a payment to eligible people, to help with some of the costs of buying continence products.