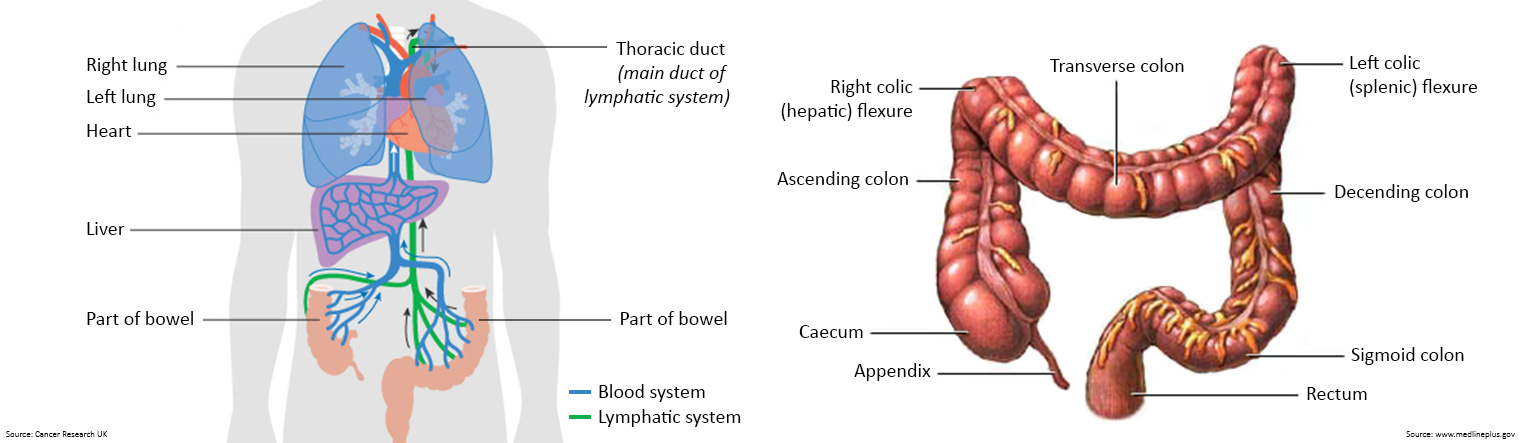
The colon is divided into four parts:
- the ascending colon is the start of the colon. It is on the right side of the abdomen. It continues upward to a bend in the colon called the hepatic flexure.
- the transverse colon follows the ascending colon and hepatic flexure. It lies across the upper part of the abdomen. It ends with a bend in the colon called the splenic flexure.
- the descending colon follows the transverse colon and splenic flexure. It is on the left side of the abdomen.
- the sigmoid colon is the last part of the colon and connects to the rectum.
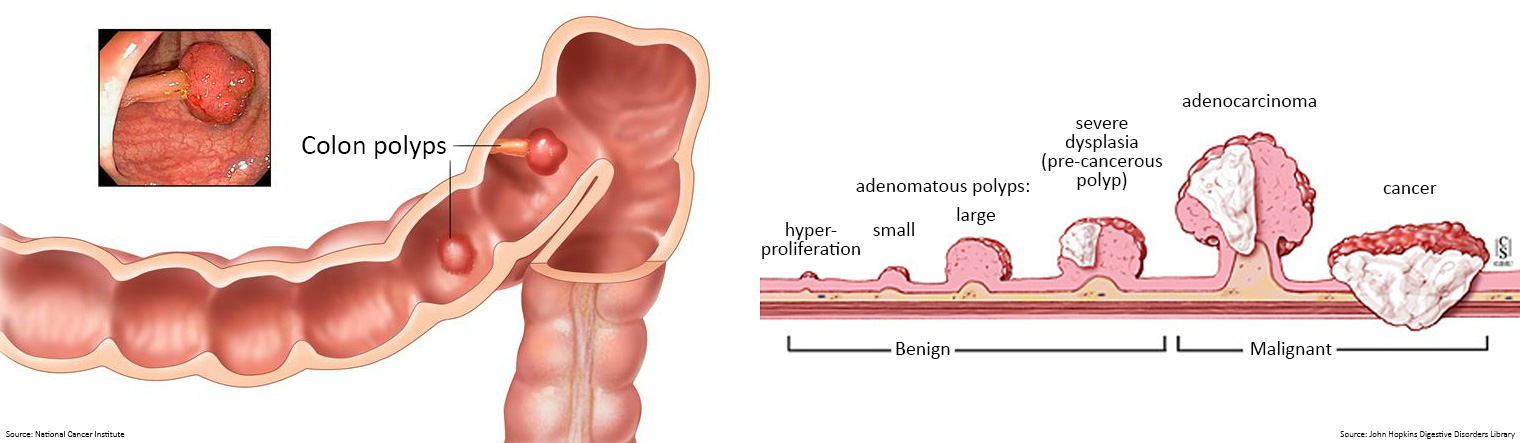
Pedunculated polyps, on the other hand, may appear raised, projecting out into the hollow centre of the bowel. They may grow in the shape of a small cauliflower or mushroom suspended from a stalk or base.
- Tubular adenomas are the most common type of bowel polyps, and usually account for 80% of all adenomatous polyps. Tubular adenomas are typically small pedunculated polyps, less than 1.2 centimetres in size. They usually have a tube-like or rounded shape. Tubular adenomas generally take years to form. Typically, the larger the polyp, the greater the risk it may become cancerous.
- Villous adenomas are generally larger pedunculated polyps and grow in a cauliflower-like shape. The term 'villous features' refers to the finger-like or leaf-like projections. Villous adenomas are more likely to become cancerous. They account for 5-15% of all adenomatous polyps.
- Tubulovillous adenomas contain a mixture of tubular and villous growth. They usually have 25-75% villous features, and they account for roughly 5-15% of all adenomatous polyps.
- Serrated adenomas contain tissues with a sawtooth look. There are two types: sessile serrated adenomas and traditional serrated adenomas. Most serrated adenomas are sessile and resemble small raised bumps. Sessile serrated polyps tend to carry a low risk of becoming cancerous as long as they do not contain major cellular changes. Traditional, or non-sessile, serrated adenomas are rarer and typically pedunculated. They carry a high risk of becoming cancerous.
- Hyperplastic polyps are typically benign, and they are not usually a cause for concern. They will rarely become cancerous, as they have a low malignancy potential.
- Inflammatory polyps occur most often in people with inflammatory bowel disease, such as Crohn’s disease or ulcerative colitis. Some people may also refer to these as pseudopolyps, as they are not true polyps but a reaction to inflammation in the colon. Inflammatory polyps are usually benign and generally do not carry the risk of developing into bowel cancer.
| Who gets bowel cancer?
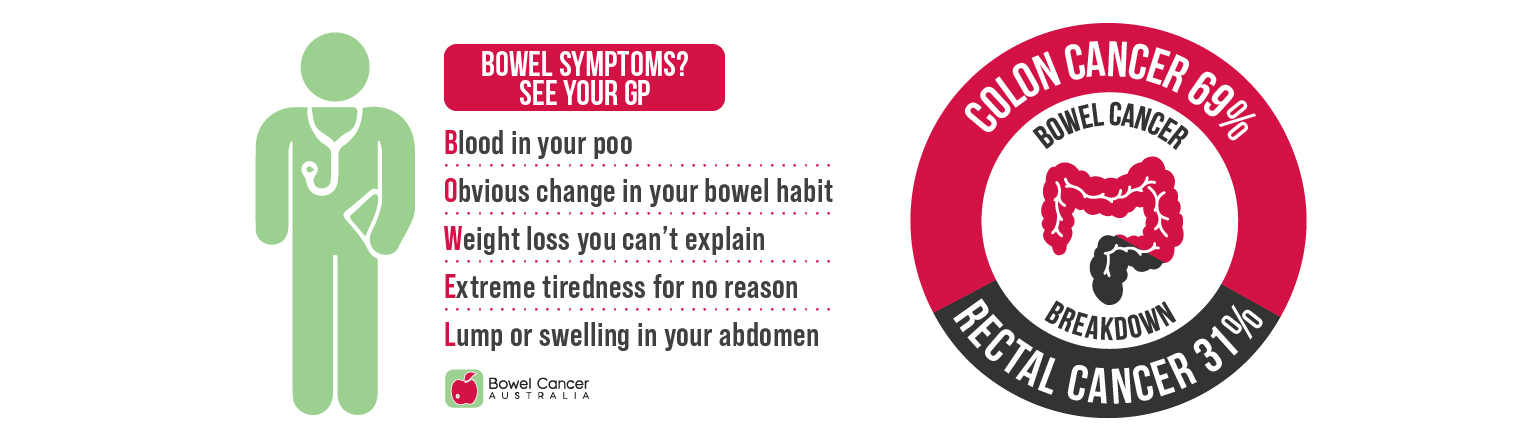
- Blood in your poo or rectal bleeding
- A recent, persistent change in bowel habit (e.g. diarrhoea, constipation or the feeling or incomplete emptying)
- A change in the shape or appearance of your poo (e.g. narrower poos or mucus in poo)
- Abdominal pain or swelling
- Pain or a lump in the anus or rectum
- Unexplained anaemia causing tiredness, weakness or weight loss
Bowel Cancer Australia recommends participating in screening appropriate to your personal level of risk.

| What is a colonoscopy?


- avoid potential adverse effects from ineffective treatments
- avoid delay in seeking alternative treatments which may be effective
- reduce the costs of ineffective treatment.
{grebox}
{/grebox}


{grebox}
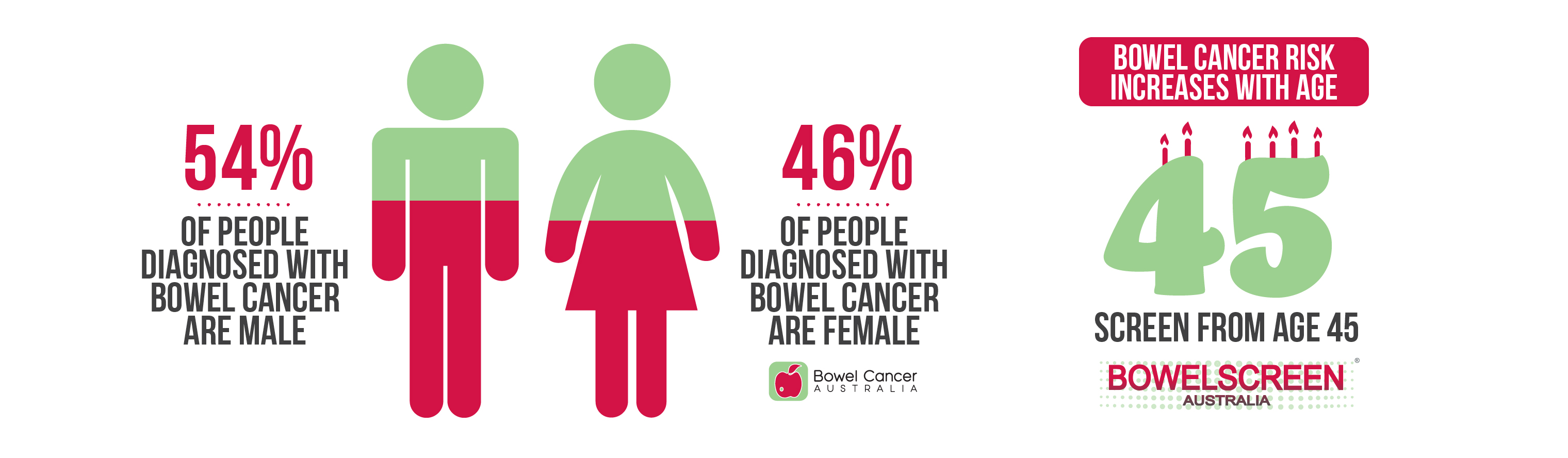
- 1 in 15 Aussie women will develop bowel cancer in their lifetime.
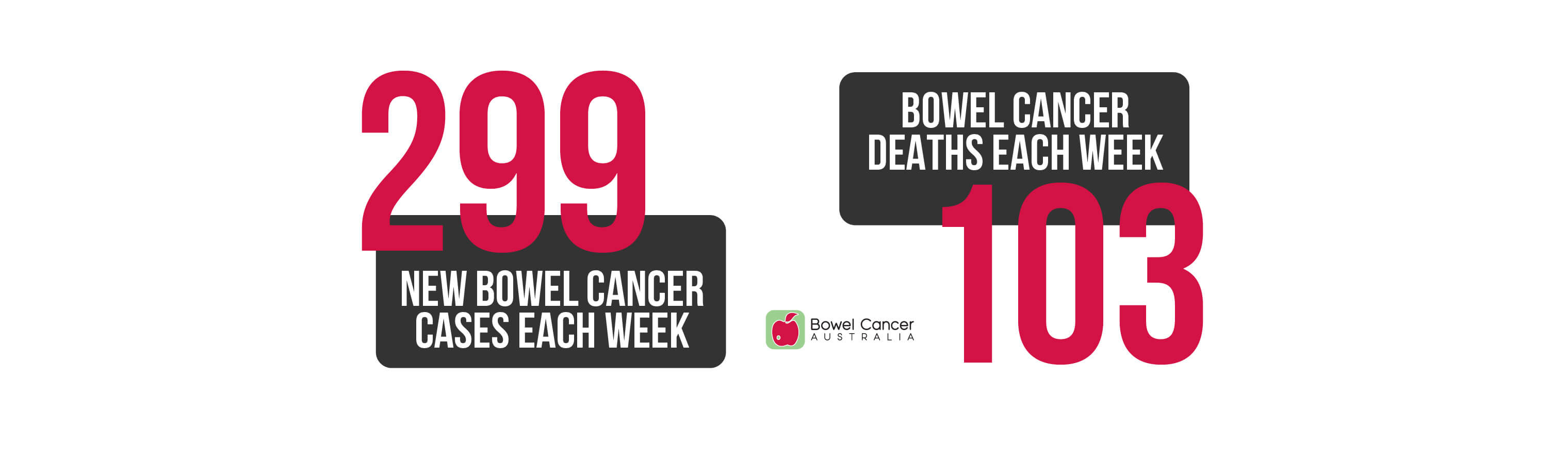
- Around 7,068 women are diagnosed with bowel cancer each year, including 872 (12.3%) under age 50.
- Bowel cancer is the third deadliest cancer in women, claiming 2,512 lives each year, including 156 (6.2%) under age 50.
- Around 45.5% of all Australians diagnosed with bowel cancer are women of all ages.
{/grebox}




- Let go of who you think you should be, who you used to be and allow yourself to embody and live life with the new changes in your body
- Practice gratitude, every day. List 3 things you are grateful and WHY (the why connects you to the feeling of gratitude)
- Mirror work every day, stand in front of the mirror and appreciate how amazing your body is, forgive it, thank it and love it. (This may be confronting, but so healing)
- Journal your thoughts, brain dump all your worries, anxieties and fears its always better out than in
- Write yourself a love letter
Empowering advice through lived experience
“Don't hide your scars. Use them for strength, use them to remember how amazing your body is and what it is capable of. Welcome the questions....open the conversation about bowel cancer and help to raise awareness and remove the stigma associated with it. I’m proud of my scars.” ~ Shannon
“Your body will change, and change forever. But this change will save your life. The change sucks but you adapt to it and fit life in your new body. Love your body and it’s new way bowel cancer treatments make it!” ~ Shelley
“It is completely valid to grieve your pre-cancer body but try not to make comparisons to your new body. It took me time to accept the changes chemo and surgery caused, but over time I’ve grown to love my scars that represent what I’ve overcome.” ~ Sofiah

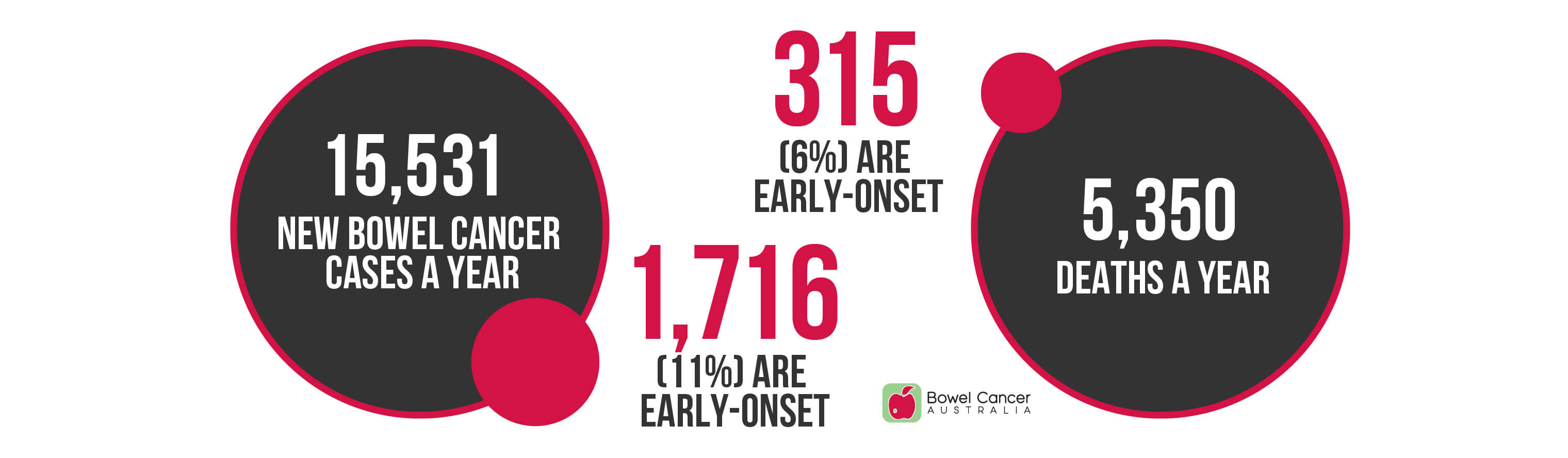
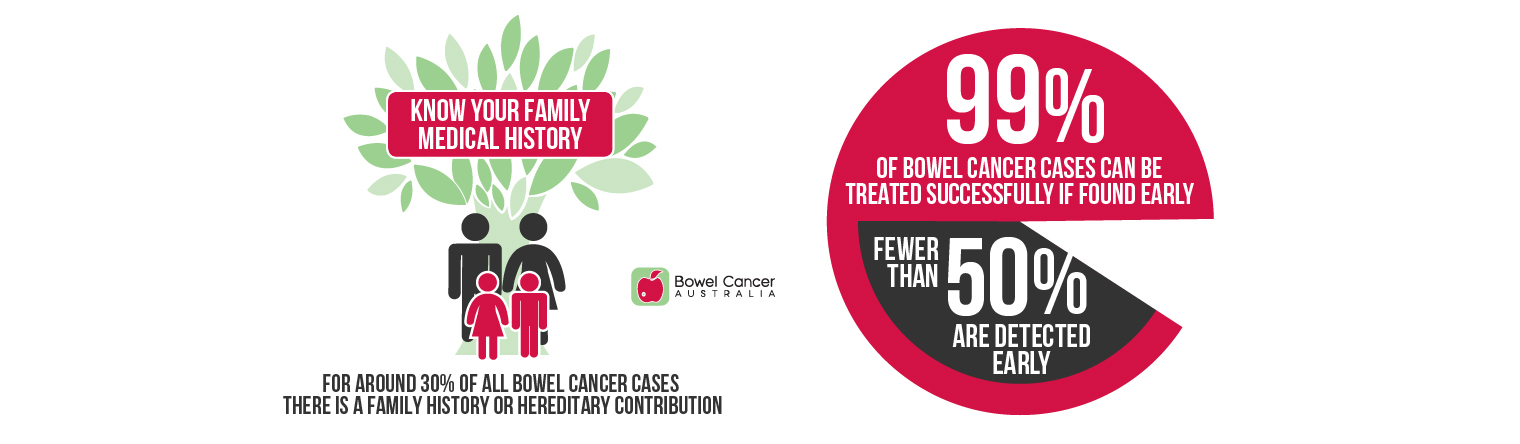
But the good news is that almost 99% of bowel cancer cases can be successfully treated when detected early.
That's why Bowel Cancer Australia is calling on all Aussie women to help us kick bowel cancer’s ass!
{grebox}
- 1 in 13 Aussie men will develop bowel cancer in their lifetime.
- Around 8,463 men are diagnosed with bowel cancer each year, including 844 (10%) under age 50.
- Bowel cancer is the third deadliest cancer in men, claiming 2,838 lives each year, including 159 (5.6%) under age 50.
-
Around 54.5% of all Australians diagnosed with bowel cancer are men of all ages.
{/grebox}


Bowel cancer treatment can come with fertility risks and understanding the preservation options available is an important consideration for many bowel cancer patients.
Just as all other side effects are discussed, possible impacts on fertility should be part of any discussions with your treating specialist before starting treatment for bowel cancer.
Men who receive a bowel cancer diagnosis before beginning or completing their families will often have many questions about how cancer treatment will affect their ability to have children in the future.
Bowel Cancer Australia has put together some helpful information about how bowel cancer surgery and treatment can affect reproductive health, what options exist to help preserve fertility before treatment begins, and what alternatives can be considered for building a family after treatment ends.
Fertility
Some treatments for bowel cancer carry a risk of infertility for women and men. Your specialist should discuss this risk with you when you are diagnosed.
Even if you’re not ready to have a child now, you might want the option to begin or grow your family in the future. Coping with a cancer diagnosis as well as possible infertility can be hard. You might feel that things are moving very quickly with little time to make important decisions. Your specialists can refer you to a counsellor or a fertility specialist.
Fertility in men
Surgery can cause erection and ejaculation issues and so may affect your fertility. Radiotherapy to the area between the hips (pelvis) usually causes infertility.
Chemotherapy can cause your body to slow down or stop the production of sperm. This can be temporary or permanent, depending on the drug and the dose. If it is temporary, sperm production can take several years to fully recover. If you are having more than one chemotherapy drug, you are more likely to have a low sperm count or stop producing sperm completely.
You will be offered the chance to store some sperm before you start your treatment, and your specialist can tell you more about this.
When to talk to your specialist about your fertility
Although you can talk to your specialist about your fertility concerns anytime, it is best to discuss them early during diagnosis and treatment planning, and before you start any treatment. This allows time for referral to a fertility specialist to learn about your risk of infertility and pursue fertility preservation, if you desire.
Contraception

A number of men living with or beyond bowel cancer and their loved ones have shared their empowering stories, you can read their Me, My Decembeard and Why stories here.
Become the face of Decembeard Australia!
Would you like to share your bowel cancer story to help raise awareness of bowel cancer in men?
To help challenge misconceptions associated with bowel cancer we need your help to spread the word!
Whether you are living with bowel cancer, beyond bowel cancer or know someone who is, we want to hear from you!
To share your story and upload a photo, please click here.
{grebox}
{/grebox}
Never2Young is an initiative of Bowel Cancer Australia, providing resources uniquely designed for younger people. Helping younger Australians to better understand their bowel cancer risk and to take appropriate action, raise much-needed awareness and receive dedicated support that is tailored to the needs of early-onset patients.
Factors like My Genes, My Family, My Health, My Body, My Lifestyle and My Right can all play a contributing role when it comes to bowel cancer in younger people.


- Greater awareness: among the community and health professionals of early-onset bowel cancer.
- Lower screening age: in response to the increasing rates of bowel cancer in younger people.
- Prompt GP referral: to a colonoscopy for all younger people who present with symptoms that may be consistent with bowel cancer.
- Improved pathways: that ensure timely triage, diagnosis and treatment for younger people.
- Better understanding: the challenges of early-onset bowel cancer to improve and tailor treatment, support and care for younger patients.
- Further research: into the causes of early-onset bowel cancer, that has the potential to improve survival and/or help build a path toward a cure.
Help us to challenge perceptions and create a powerful voice for change by sharing our Never2Young Advocacy Agenda and your lived experience.
{grebox}
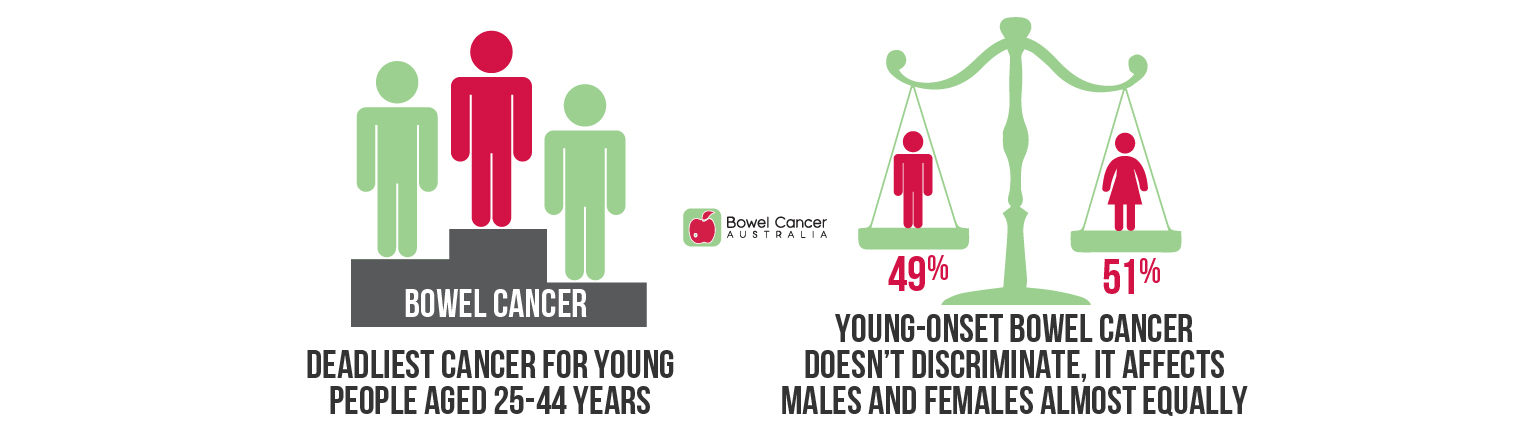
- 1,716 Australians under age of 50 are diagnosed with bowel cancer each year (11% of all bowel cancer cases).
- 315 people under age 50 die from bowel cancer each year (5.8% of all bowel cancer deaths).
- 50.8% of early-onset bowel cancer cases are diagnosed in females, and 49.2% in males.
- Over 86% of people diagnosed with early-onset bowel cancer experience symptoms.
{/grebox}
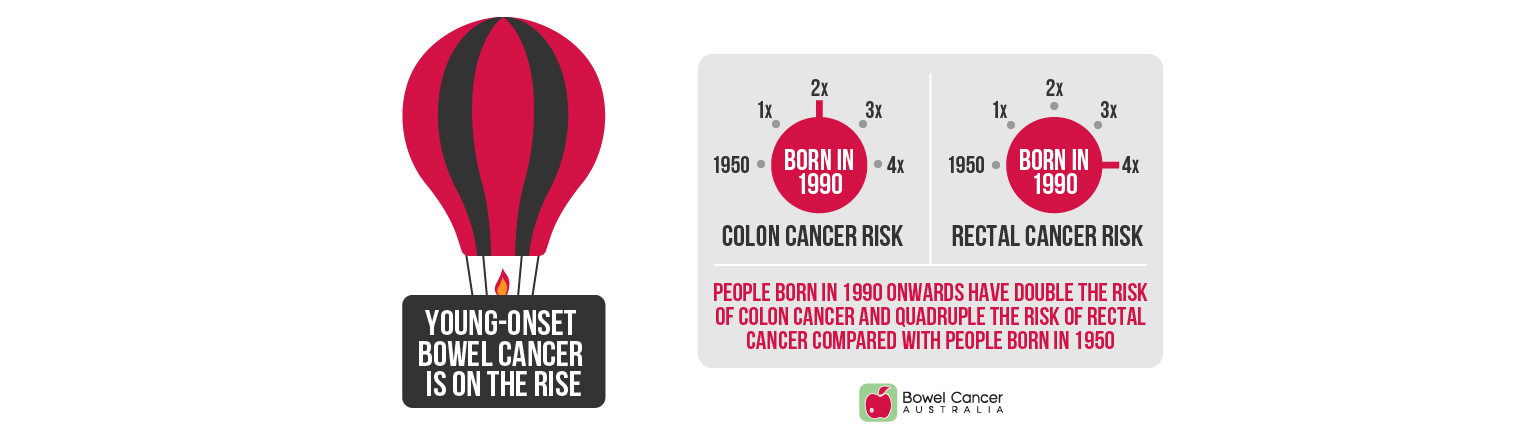
People born in 1990 onwards have double the risk of colon cancer and quadruple the risk of rectal cancer compared with people born in 1950.
{grebox}
- Over the past three decades there has been a 266% increase in bowel cancer incidence rates in adolescents and young adults (15-24 years).
- Bowel cancer is the fifth most common and seventh deadliest cancer for people aged 15-24.
- The proportion of bowel cancer located in the appendix was 85% for people aged 15-24 compared to only 3% for people older than 24.
- More females than males aged 15-24 developed bowel cancer.
- The five-year relative survival for people aged 15-24 was 96% (2014-18), which means adolescents and young adults have around a nine in ten chance of surviving five years after diagnosis relative to comparable people in the general population.
{/grebox}
Although many of the symptoms of bowel cancer are common to multiple health concerns, please do not accept "you're too young to have bowel cancer" as an explanation for your symptoms, ask your doctor to be referred for further investigations.
Published in the ANZ Journal of Surgery (8 June 2020), a Gold Coast study found growing evidence of increasing rates of bowel cancer in people under age 50 after reviewing 557 patients who received a colonoscopy between 2013 and 2017.
The findings correlate with published research in the Lancet Gastroenterology & Hepatology (May 2019), that found the number of people under age 50 diagnosed with colon (2.9%) and rectal (2.6%) cancer increasing significantly each year in Australia.
Of the top 10 cancers in Australia, bowel cancer is the only cancer that showed an increase in mortality rates from 2008 to 2018, projected to 2021 for people aged 45-49.
A 45-year-old today has the same bowel cancer risk a 50-year-old had 10 years ago.
Screening from 45 has been shown to be potentially cost-effective for the National Bowel Cancer Screening Program, would reduce the number of bowel cancer cases and deaths, and increase demand for colonoscopy services, depending on participation.
Australia can’t afford to wait another 12 years for our medical guidelines to be updated before taking action.
If you or a loved one, no matter your age, are experiencing bowel cancer symptoms, talk with your GP and advocate for your own health.
Knowing your family history is also vital. You may need to begin screening even earlier depending on your individual circumstances.
{grebox}
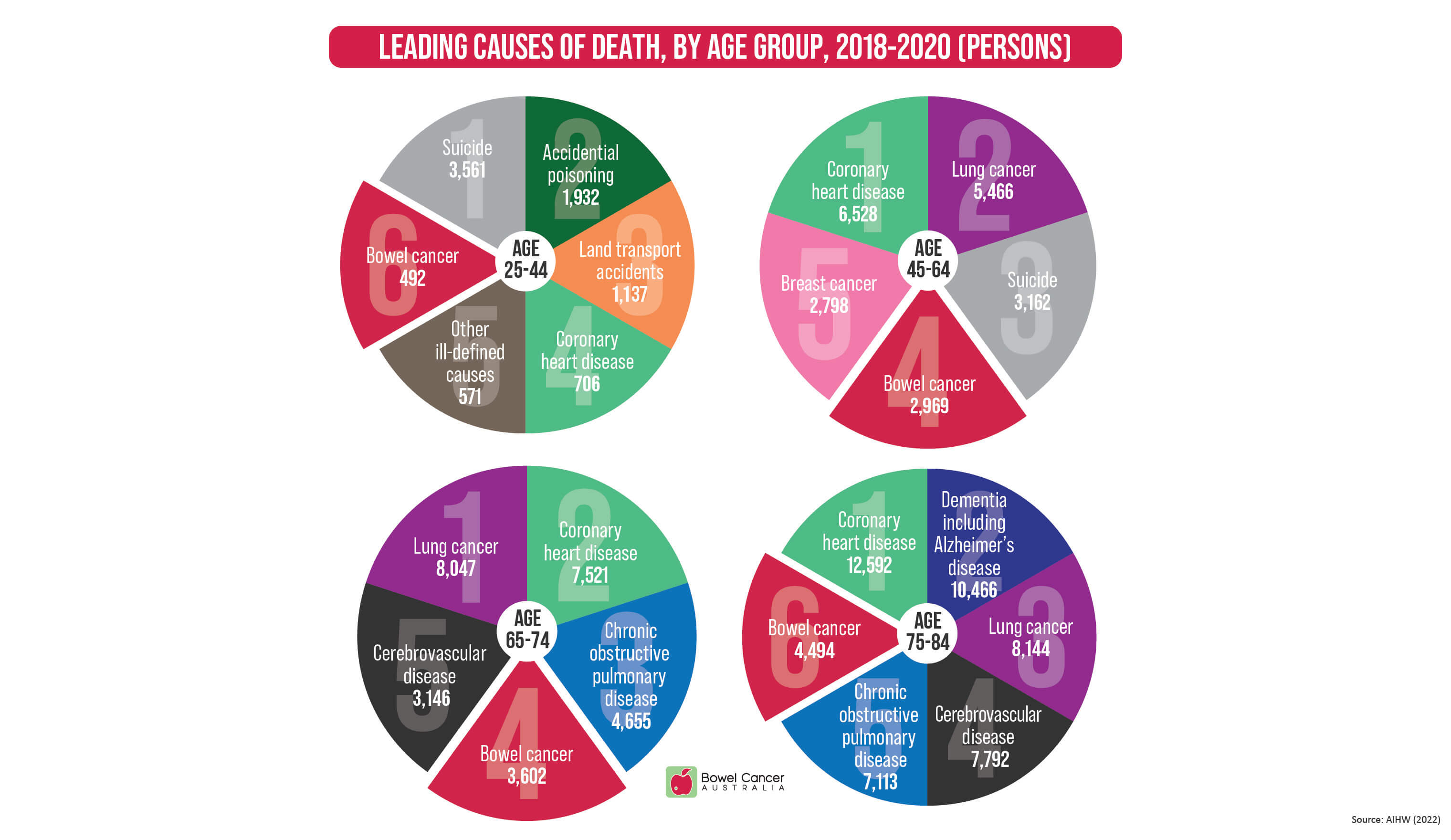
Bowel Cancer Australia recognises lowering screening guidelines is one step forward for people aged 45 and older, but it doesn’t address the rise in early-onset bowel cancer, which is now the sixth leading cause of death for Australians aged 25-44.
{/grebox}
In October 2020, the American Gastroenterological Association (AGA) published a new clinical practice update on young adult-onset bowel cancer that provides best practice advice that has been shown to work effectively and produce successful outcomes, which can be immediately implemented in patient care.
- BEST PRACTICE ADVICE 1 - With the rising incidence of people developing bowel cancer before 50 years of age, diagnostic evaluation of the colon and rectum is encouraged for all patients, irrespective of age, who present with symptoms that may be consistent with bowel cancer, including but not limited to: rectal bleeding, weight loss, change in bowel habit, abdominal pain, iron deficiency anaemia.
- BEST PRACTICE ADVICE 2 - Specialists should obtain family history of bowel and other cancers in first- and second-degree relatives of patients with young adult–onset bowel cancer and discuss genetic evaluation with germline genetic testing either in targeted genes based on phenotypic presentation or in multiplex gene panels regardless of family history.
- BEST PRACTICE ADVICE 3 - Specialists should present the role of fertility preservation prior to cancer-directed therapy including surgery, pelvic radiation, or chemotherapy.
- BEST PRACTICE ADVICE 4 - Specialists should counsel patients on the benefit of germline genetic testing and familial cancer panel testing in the pre-surgical period to inform which surgical options may be available to the patient with young adult–onset bowel cancer.
- BEST PRACTICE ADVICE 5 - Specialists should consider utilising germline and somatic genetic testing results to inform chemotherapeutic strategies.
- BEST PRACTICE ADVICE 6 - Specialists should offer hereditary bowel cancer syndrome specific screening for bowel cancer and extra-colonic cancers only to young adult–onset bowel cancer patients who have a genetically or clinically diagnosed hereditary bowel cancer syndrome. For patients with sporadic young adult–onset bowel cancer, extra-colonic screening and bowel cancer surveillance intervals are the same as for patients with older adult–onset bowel cancer.
{grebox}
The update states that the signs and symptoms that prompt healthcare providers to consider a diagnostic bowel exam for a person over 50 should prompt a diagnostic colonoscopy exam for the person under 50 years of age.
{/grebox}

Many young bowel cancer patients say that they can feel quite alone and isolated when first diagnosed with bowel cancer and during their bowel cancer journey.
Often because there is a common misconception in the community that bowel cancer only affects older people and also because many of the other bowel cancer patients they encounter during treatment are older.
Parents with young children, people just starting out in their career, singles, university students and newly-weds – younger bowel cancer patients can quite often be in a different life stage to those diagnosed at an older age.
Having a child diagnosed with bowel cancer can also be very difficult.
The ability to talk with others who know what you are going through can be very helpful, and that is what Bowel Cancer Australia's Peer-to-Peer Network is all about – connecting people living with or beyond bowel cancer and loved ones with others in a similar situation.
Sharing your story and experiences to raise awareness and help others is also a big part of Bowel Cancer Australia's Peer-to-Peer Network.
You can read the inspiring bowel cancer stories of many young bowel cancer patients and their loved ones and/or submit your story here.
| N2Y Awareness
If you are living with or beyond early-onset bowel cancer, or are a loved one, and would like to become a #N2YChampion,
please register your interest on our contact us webpage.